Marlene M. Steinheiser, PhD, RN, CRNI®, shares her personal experiences with self-advocacy in infusion therapy. As a seasoned infusion professional, Dr. Steinheiser has not only advocated for her own safety and educated the clinicians around her, but has extended her guidance to family, teaching others how to ensure they receive the best IV therapy possible.
Beginning My Journey in IV Therapy
I fondly recall graduating from nursing school in 1986 and starting my career as a float nurse in a community hospital. My nurse preceptor was nicknamed “Sarg” (short for sergeant) because she was a retired military nurse and “ran things by the book.” It was nice to have an experienced nurse with whom I could validate my practice, but as a new nurse, I also didn’t think to question what I was being taught.
For example, was it best practice and based upon current evidence? Or was it merely the way other nurses had always done things? I don’t recall knowing where I could find all the information I needed, especially since caring for patients involved wound care, IV medications, suctioning, and many other procedures.
After spending only a couple of years in acute care, I became interested in home care and was intrigued with home infusion therapy. At that time, a colleague urged me to join the Infusion Nurses Society (INS) and become certified in infusion therapy. At this point in my career, I began to realize that I had an opportunity to help other nurses remain current with best practices when placing vascular access devices for patients and administering infusion therapy.
When I became a nurse manager and eventually an educator, I stayed abreast of the INS Infusion Therapy Standards of Practice in order to guide thedevelopment of policies and procedures and to adequately mentor nurses in our organization. Evidence is always evolving, providing us with new knowledge, and thus challenging us to stay up-to-date with best practices.
Self-Advocacy
Many of us have had or will have a peripheral intravenous catheter (PIVC) inserted. Perhaps someone in your family has received infusion therapy when hospitalized, in an infusion center, or at home. I wish to share two experiences I had with PIVC insertions and infusion therapy.
Educating Through Experience:
The first experience was when I went to an outpatient center for a minor screening exam that required that I have a PIVC started. The nurse assigned to me seemed relatively young in her career. She began the procedure unsure of her knowledge and practice, which created anxiety in me. I wanted to speak up but didn’t want to be “that nurse”, the one who is supposed to be the patient but is switching to the role of nurse. I also didn’t want to make her nervous.
As I lay there in the bed, she proceeded to slap my forearm in an attempt to locate a vein. This created even more anxiety as she looked unsure of where she might attempt to cannulate my arm. Once she located an appropriate vein, she cleansed the site but decided to tap on the vein to be sure of her location. I knew then that I needed to advocate for myself, but I also found this to be an opportunity to help this nurse to understand best practice. I kindly asked her if I could help provide her with some tips.
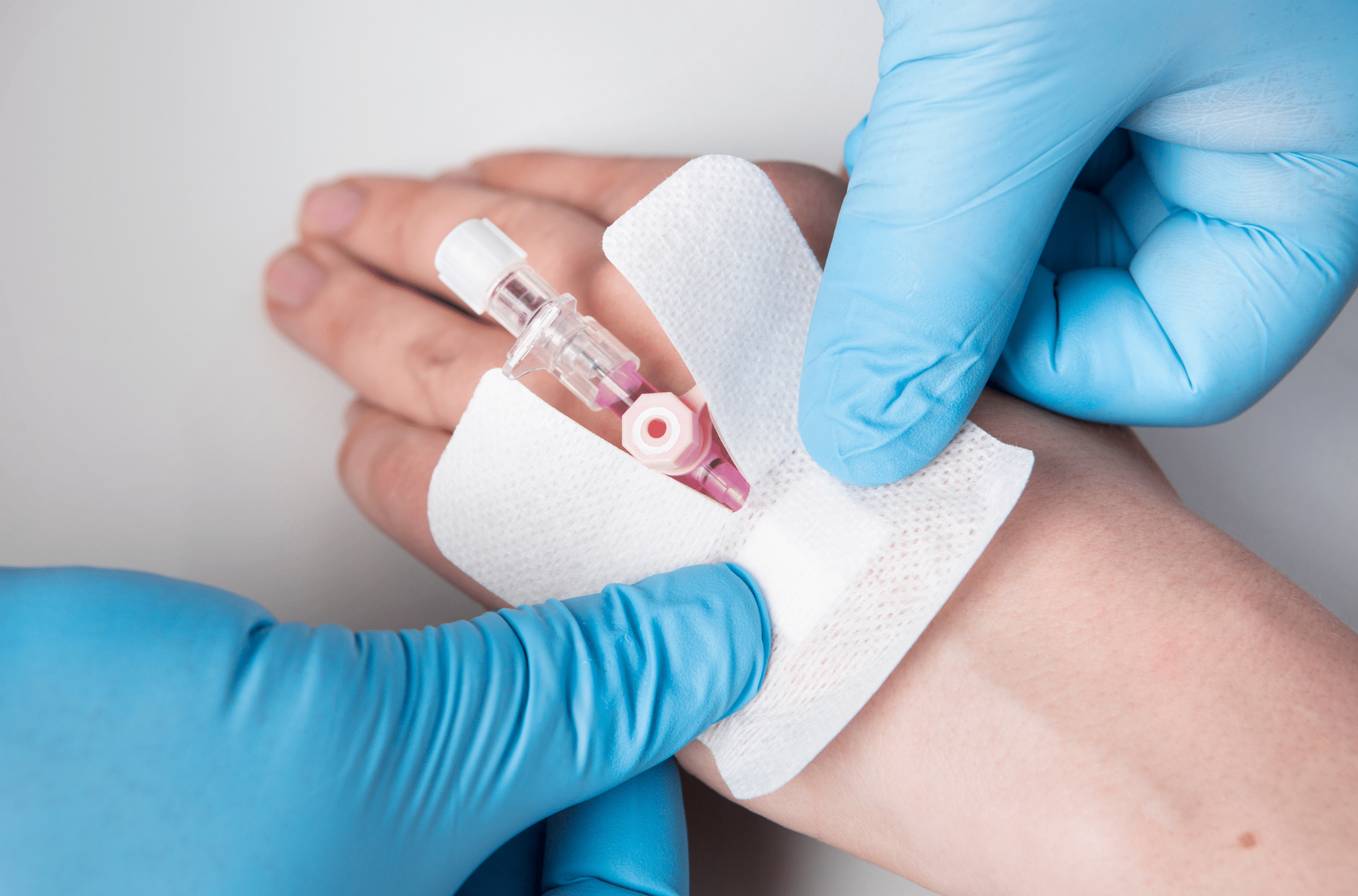
She admitted she was a new nurse and I disclosed that I was a nurse certified in infusion therapy. She was so grateful and said no one had ever really taught her how to properly assess a patient for PIVC insertion. She also did not realize that after cleansing the site that she should not have re-palpated it. At that moment, she expressed her appreciation for my sharing of best practices. It was a win-win!
Insertion of PIVCs seems harmless to most and without too many risks. However, PIVCs carry significant patient risks such as infection, infiltration, phlebitis, and nerve damage. I was grateful to have the opportunity to mentor a nurse who wanted to provide me with the best care possible but just did not know how. One nurse, one IV at a time.
Best Practices in Action
My second experience was a bit different, although also in an outpatient setting. This time the nurse who was placing my PIVC felt fairly confident that she could cannulate the vein of choice but still had some doubts due to my overnight NPO status. 
As we both looked at my forearm, I shared with her the location that usually works well but also mentioned that it seemed less prominent given my slight dehydration. She looked at me and said, “I’ll be right back.” She came around the corner with a near-infrared vein visualization device which she used to swiftly place my PIVC. I was relieved!
Best practice is to use available visualization technology to confirm the vascular access site when necessary. How did she learn to assess using vein visualization technology? If anesthesia hadn’t come into my room right after that and put me in a “happy place,” I would have asked. But as a patient, I appreciated her commitment to my comfort and care by keeping up-to-date with best practices and new evidence.
Teaching Family to Be Self-Advocates
As most nurses know, when you are the nurse in the family everyone calls you to ask about what ails them. But because both of my parents have been in and out of acute care and outpatient facilities over the years, I have taught them a bit about infusion therapy so they can be self-advocates. At the very least, they know when something does not seem right, and they give me a call.
 One day my mother called me and said, “Your dad is in the emergency department.” She said they placed a PIVC in his antecubital space and another in his hand. When I talked to my dad, he said he kept getting the IV in his hand wet when he washed his hands, and he knew that this did not seem right.
One day my mother called me and said, “Your dad is in the emergency department.” She said they placed a PIVC in his antecubital space and another in his hand. When I talked to my dad, he said he kept getting the IV in his hand wet when he washed his hands, and he knew that this did not seem right.
My mom sent me pictures once he arrived at the unit for his planned inpatient stay, and by this time, I learned my dad was due for a contrast dye study via one of these PIVCs which was placed a couple days prior. Advocating for my dad when I was almost 2,000 miles away would have been a challenge, if not for my mom who had learned enough to understand that PIVCs placed in those areas were not optimal and possibly an extravasation risk for a contrast dye study.
After another discussion with me, she called my dad’s nurse into the room requesting those PIVCs be discontinued, and that a new site be used for his PIVC. I soon received a lovely photo of a PIVC placed in my dad’s forearm with a picture perfect IV dressing. And guess what? He only needed one of those PIVCs after all.
Key Takeaways
- The role of a nurse is complex.
- There is much to learn as a new nurse, and we ALL continue to evolve in our practice.
- Nurses want to provide optimal patient care.
- Nurses need access to evidence-based resources to support their learning.
- Nurses are wonderful patient advocates.
The complex treatment of infusion therapy is constantly evolving, and the implementation of best practices protects our patients from harm. Infusion therapy encompasses a wide range of vascular access devices, procedures, IV therapies, and medications. How can we keep up-to-date with the evidence relating to peripheral catheter bundles, the risks involving IV Push medications, peripherally inserted central catheters, or administration of hazardous drugs?
Challenge yourself to continue your own education about best practices so you can provide optimal patient care and be the best advocate for your patients.