Infusion Nurses Society (INS) Nurse Educator Derek Fox, MSN, RN, VA-BC, CRNI®, NEA-BC and Director of Clinical Education Marlene Steinheiser, PhD, RN, CRNI® join us to discuss the importance of continuing education (CE) for the nursing practice, including its benefits for clinicians, common barriers to learning, and available educational resources provided by INS.
Nursing practice is constantly evolving due to ongoing research advancements and the emergence of new technologies. In a few short decades, the nursing profession has gone from Rolodex, paper charts, and gravity-run infusions to intranet directories, electronic health records, and smart infusion pumps. These are just a few examples, but to the point, it is easy to see how these quick advancements have shaped nursing.
This progression has enabled the profession to increase efficiency, eliminate tasks, and enable quick and concise communication. For some, it may be difficult to imagine a time that solely relied on printing releases, in-person meetings, and most communication being face-to-face. Like many of the nursing domains that became more efficient, evidence-based practice (EBP) accelerated.
With the increase in efficiency of research, peer-review methods, and consensus came the more frequent changes in standards, guidelines, policy, and law.
What is EBP without dissemination? This question guides our thinking to understand the importance of continuing education to ensure our professional practice is reflective of best patient outcomes. The pursuit of education and lifelong learning is highly valued by many, but some report downward trends in nursing certification, continued education participation, and an overall perspective shift.
How does the nursing profession address this, and why should this be prioritized? This answer is influenced by technological advancements, shifts in nursing culture, the development of new nurse cohorts, changes in resource policies, and the promotion of transformational leadership exemplars.
While the state of commitment to lifelong learning is constantly changing, there is one strategy that has shown success through all these transitions. That constant is meeting the learner where they are, but where are the nurses currently?
What’s in it for ME (WIIFM)?
To meet nurses where they are requires an understanding of their motivations, goals, and interests. WIIFM is a popular acronym used to describe the motivating factors that facilitate change, foster healthy communication, and even leverage marketing strategies. It has been widely accepted across the spectrum of professions both in and out of health care. These concepts are based upon the key principles of self-determination theory, Maslow’s Hierarchy of Needs, Cialdini’s Principles of Influence, and behavioral economics. 1-4
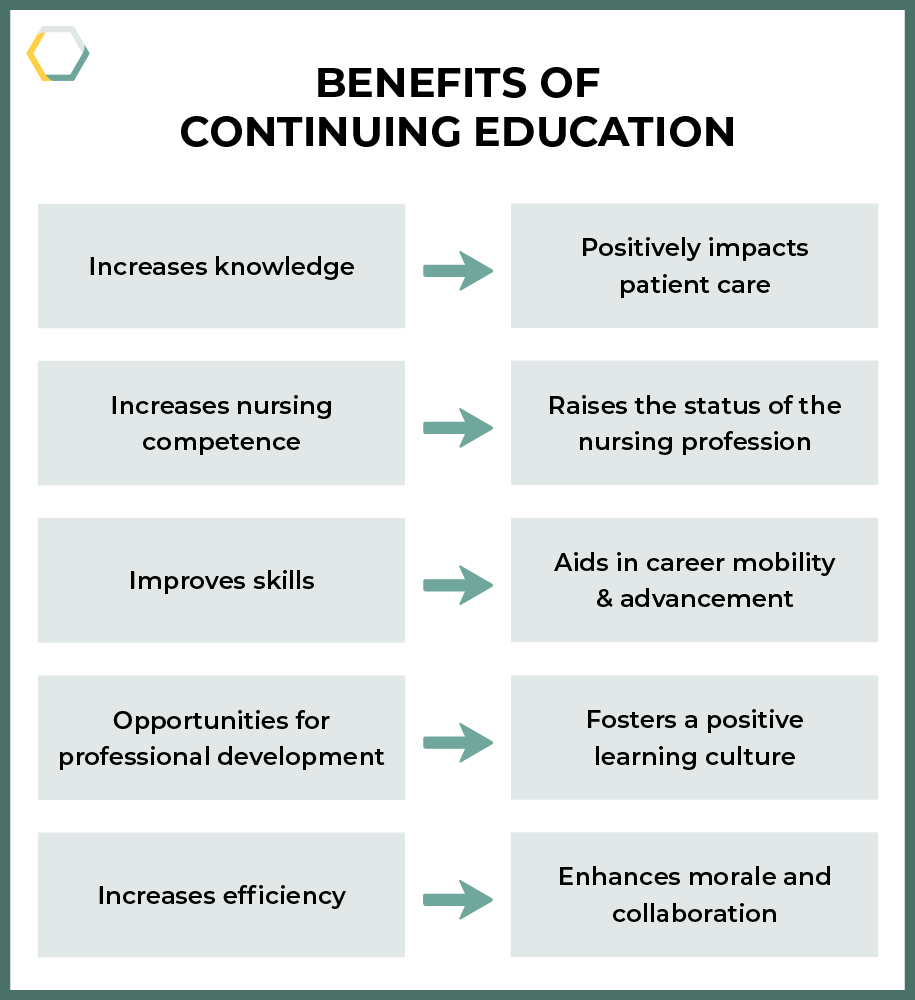
In nursing professional development, WIIFM can be applied by answering the question, “So, what does continuing education (CE) have in it for nurses?”
-
CE increases knowledge and competence. This, in return, has positive impacts on patient care. 5
-
Increased nursing competency raises the status of the profession. 5
-
Skills and knowledge gained through CE can aid in career mobility and advancement.
-
Some organizations offer career portfolio programs and clinical ladders that provide financial incentives to nurses who work on their personal professional development.
-
Professional development enhances the working environment by contributing to a positive learning culture.
-
Increased efficiency of nursing teams enhances increased morale, creativity, satisfaction, collaboration, and communication.
Overcoming Barriers to Continuing Education
Barriers are evident, and increases in these barriers continue to contribute to the downward trend in continuing education. Nurses indicate that the largest influences in attitudes toward CE are organization culture, supportive environments, nurses’ perception of barriers, perceived impact on practice, and financial restrictions. 5,6
Policies on continuing education for nurses vary widely. Some states have progressive policies mandating continuing education, while others have no such requirements. Is requiring continuing education an effective approach?
Leadership
Transformational leadership plays a pivotal role in fostering a positive attitude toward continuing education. Leaders who inspire and motivate their teams can create an inclusive and encouraging environment that enhances job satisfaction and professional growth. 7 Reflecting on leadership styles and their impact on promoting education is crucial for all nursing leaders.
Financial Restrictions
Another concern is budget cuts associated with a decreased education allowance for nurses in many organizations. These financial constraints limit nurses’ access to quality education, which is essential in maintaining high standards of care. While some non-profit organizations provide funding, many nurses feel obtaining quality continued education is out of their reach due to the associated costs.
When addressing these barriers, a multifaceted approach is needed.
Transformational Leadership: Leaders should adopt leadership styles that inspire and motivate their teams.
Financial Support: Increase funding by grants, increase budgets allowing for CE expansion, and gain non-profit support.
Cultural Shift: Promote a culture that values and prioritizes lifelong learning.
INS: SETTING THE STANDARD FOR INFUSION CARE™️
At the Infusion Nurses Society (INS), the education department identifies the needs of learners by collecting data from continuing education evaluations, collaborating with experts, and identifying industry trends. INS makes it a priority to contribute to the dissemination of new evidence, provide pertinent updates to clinicians, and address key concerns within the specialty of infusion therapy.
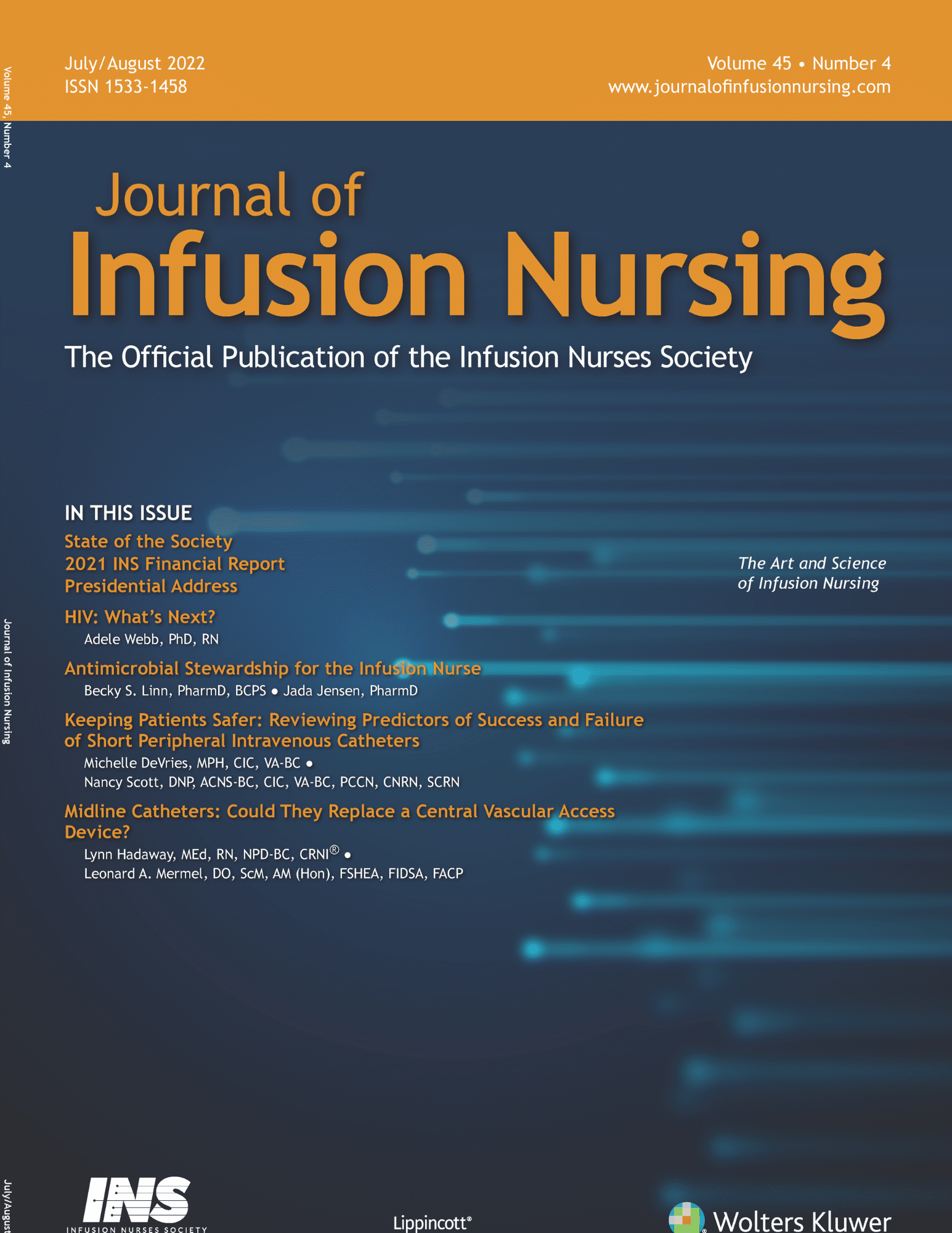 INS appeals to all learner types with a wide range of offerings,8 including in-person/virtual (hybrid) annual meetings, virtual symposiums, webinars, podcasts, the Journal of Infusion Nursing, the INSider newsletter, artificial intelligence (AI) technology referencing the INS Infusion Therapy Standards of Practice, 9 and social media. Each learning asset is designed to engage a specific learner type, making the education content engaging for all learners.
INS appeals to all learner types with a wide range of offerings,8 including in-person/virtual (hybrid) annual meetings, virtual symposiums, webinars, podcasts, the Journal of Infusion Nursing, the INSider newsletter, artificial intelligence (AI) technology referencing the INS Infusion Therapy Standards of Practice, 9 and social media. Each learning asset is designed to engage a specific learner type, making the education content engaging for all learners.
INS Continuing Education Exemplar
To better understand the value and need of continuing education, consider the following exemplar of recent new guidance and take a closer look into the INS Standards of Practice. 9 INS education is based upon the Infusion Therapy Standards of Practice (Standards). The Standards provide nurses and all clinicians who provide care for patients with vascular access devices receiving infusion therapy with evidence to support their practice. 
Vesicant medications and solutions are addressed throughout various aspects of infusion therapy statements in the 2024 Standards. Recent evidence has led to changes in practice related to short-term, temporary infusion of vasopressors (a vesicant) via a short peripheral intravenous catheter (PIVC). As practice has evolved, so has the need for further education and research about vasopressor administration via PIVCs.
The INS Standards state the following regarding use of PIVC to infuse vesicants and irritants:
- “Avoid use of a short PIVC for continuous infusion of medication with irritant or vesicant properties. For time-critical infusions (eg, vasopressors), consider the type and dose of medication and its mode of action (vasoconstriction vs vasodilation). Where appropriate, begin the infusion through a PIVC. The PIVC should be replaced with a central venous access device (CVAD) as early as possible, balancing the acuity of the patient and the potential harm of peripheral infusion of peripherally incompatible medication.”
- “Increase catheter site surveillance when administering intermittent infusions for any duration of known irritants and vesicants due to increased risk of phlebitis or extravasation.” 9(S87)
- “Recognize the differences between vesicant, nonvesicant, and irritant solutions and medications. Each organization should reach a consensus on what medication is a vesicant and irritant based on their internal formularies and the populations they serve.” 9(S155)
Nurses may ask, what is a vesicant? How can nurses find out information about infusion of vesicants? When turning to INS to answer this question, here are a few available resources the nurse may utilize to answer this question.
- ASK IVY ™: One way is by using the INS
 feature ASK IVY ™.10 Powered by AI and aligned with the Infusion Therapy Standards of Practice, 9th edition,9 ASK IVY ™ is a go-to resource for answers to clinical questions. Ivy answers the question, “what is a vesicant?” with “A vesicant is a type of medication or solution that can cause tissue damage and blistering if it leaks out of the vein into the surrounding tissue, a process known as extravasation. Vesicants are often used in chemotherapy and require careful handling and administration to prevent injury.”
feature ASK IVY ™.10 Powered by AI and aligned with the Infusion Therapy Standards of Practice, 9th edition,9 ASK IVY ™ is a go-to resource for answers to clinical questions. Ivy answers the question, “what is a vesicant?” with “A vesicant is a type of medication or solution that can cause tissue damage and blistering if it leaks out of the vein into the surrounding tissue, a process known as extravasation. Vesicants are often used in chemotherapy and require careful handling and administration to prevent injury.” - Journal of Infusion Nursing: The nurse may further ask after using ASK IVY ™, “How do I know specifically which agents are vesicants?” To assist clinicians in their continuing education about vesicants, INS convened a Vesicant Task Force who, in September 2024, published the Development of an Evidence-Based List of Non-Antineoplastic Vesicants: 2024 Update.11 This guidance document offers a tool for categorizing risks by level, tables outlining vesicants with moderate-to-high risk, a cautionary list of vesicants, an evidence-based table for administering vasopressors through peripheral intravenous lines, and a checklist for preventing extravasation.
- Virtual Symposium: Prior to the 2024 publication, INS conducted a five-session virtual symposium to guide clinicians who are administering or ordering vesicant agents.
- Webinar: At the time of publication in September 2024, INS provided a one-hour webinar specifically addressing the complications of extravasation of these agents.9
So, let’s take this exemplar back to the topic of WIIFM. As nurses, we are empowered with knowledge to advocate for our patients. For instance, when you know which agents are vesicants, you can advocate for the most appropriate vascular access device, understand the administration risks, how to recognize complications, and intervene in a timely manner.
The act of patient advocacy builds trust and enhances patient safety. Knowledge of current evidence and best practices can also protect the nurse while adhering to the current Standards. Consider your role as a mentor for others as you share your knowledge and resources with other nurses or clinicians. Finally, exercise the ability to advocate for yourself, friends, or loved ones when they are receiving infusion therapy and, in this case, a vesicant agent.
Real-life Application
I, Marlene, can personally relate to this education exemplar in many ways. When my father was hospitalized with a three-day-old PIVC placed in his hand, he called me and said, “I am hitting my IV on the sink and getting it wet while I am using the bathroom.”
He added that they were taking him for an MRI with contrast media. This agent is listed as a high-risk vesicant that can result in extravasation, leading to severe complications, including tissue death, amputations, and other permanent damage.10
Knowing the associated risk and the condition of his current PIVC, I assisted him to advocate for placement of a new PIVC prior to his MRI study to ensure safe administration of a known vesicant.
As I prepare for my own upcoming MRI with contrast dye, I plan to self-advocate to visualize a brisk, red blood return prior to dye administration to confirm PIVC patency. And when teaching other nurses through presentations and publications, I feel I am empowering them to protect patients from harm and build trust. This provides a sense of commitment to our profession and a way of giving back.
Summary
Continuing education can be delivered in various forms, and individual preferences for delivery may vary depending on the topic, cost, and time available for the education. Build passion for your work by sharing what you have learned with other nurses or clinicians and educate patients so they may be self-advocates. Be a role model for others demonstrating what you have learned.
We engage in continuing education because we care. We care about our patients, our friends, our loved ones, and ourselves. Find your passion for continuing education and share it with those around you! You may never know the lives you can impact because of what you have learned.
1 Cialdini RB. Influence: Science and Practice. 4th ed. Allyn & Bacon; 2001.
2 Deci EL, Ryan RM. The “what” and “why” of goal pursuits: human needs and the self-determination of behavior. Psychol Inq. 2000;11(4):227-268. doi.org/10.1207/S15327965PLI1104_01
3 Kahneman D, Tversky A. Prospect theory: an analysis of decision under risk. Econometrica. 1979;47(2):263-291. doi.org/10.2307/191418
4 Maslow AH. A theory of human motivation. Psychol Rev. 1943;50(4):370-396. doi.org/10.1037/h0054346
5 Mlambo M, Silén C, McGrath C. Lifelong learning and nurses’ continuing professional development, a metasynthesis of the literature. BMC Nurs. 2021;20(1):62. doi.org/10.1186/s12912-021-00579-2
6 Kurtović B, Gulić, P, Čukljek S, Sedić B, Smrekar M, Ledinski Fičko S. The commitment to excellence: understanding nurses’ perspectives on continuous professional development. Healthcare (Basel). 2024;12(3):379. doi.org/10.3390/healthcare12030379
7 Steinmann B, Klug HJP, Maier GW. The path is the goal: how transformational leaders enhance followers’ job attitudes and proactive behavior. Front Psychol. 2018;9:2338. doi.org/10.3389/fpsyg.2018.02338
8 Infusion Nurses Society. (2024). INS Learning Center. INS. Accessed October 8, 2024. https://www.learningcenter.ins1.org/
9 Nickel B, Gorski LA, Kleidon TM, et al. Infusion therapy standards of practice, 9th ed. J Infus Nurs. 2024;47(Suppl 1):S1-S285) doi:10.1097/nan.0000000000000532.
10 Infusion Nurses Society. ASK IVY. Accessed October 1, 2024. https://www.ins1.org/ask-ivy/
11 Gorski LA, Ong J, Van Gerpen R, Nickel B, Kokotis K, Hadaway L. Development of an evidence-based list of non-antineoplastic vesicants: 2024 update. J Infus Nurs. 2024;47(5):290-323. doi.org/10.1097/NAN.0000000000000568
 Derek Fox, MSN, RN, VA-BC, CRNI®, NEA-BC, is the Infusion Nurses Society (INS) Nurse Educator, dedicated to advancing clinical excellence in infusion and vascular access. With extensive experience as a clinician, leader, and educator, Derek helps shape the future of infusion practice. He collaborates with esteemed professionals to produce high-quality education sessions at the INS annual meeting, webinar opportunities, and hosts the INS podcast that is set to relaunch soon.
Derek Fox, MSN, RN, VA-BC, CRNI®, NEA-BC, is the Infusion Nurses Society (INS) Nurse Educator, dedicated to advancing clinical excellence in infusion and vascular access. With extensive experience as a clinician, leader, and educator, Derek helps shape the future of infusion practice. He collaborates with esteemed professionals to produce high-quality education sessions at the INS annual meeting, webinar opportunities, and hosts the INS podcast that is set to relaunch soon.