In this RxToolKit article, Katie Nesbitt, PharmD, BCPS introduces intravenous therapy, the conditions it treats, and why someone might choose this method of administration. She also explores the different types of vascular access devices, considerations for medication administration, complications associated with VADs and their management, and the pharmacist’s role in the management of VADs.
What is intravenous therapy?
Intravenous (IV) therapy is the method of supplying medications, fluids, blood products, or nutrition to the body via the veins. Using a soft, flexible tube inserted into the vein, an IV provides a regulated amount of a product into the bloodstream.
Intravenous infusion was first documented in the 15th century when a doctor attempted a blood transfusion between three boys and Pope Innocent VIII. While this attempt ultimately failed, experiments with intravenous therapy for health benefits continued into the present day, when they can successfully save lives and improve the quality of life for countless individuals.
What does IV therapy treat?
There are many different types of IV infusions used to address different needs. These include chemotherapy, immunotherapy, fluids, antibiotics, nutrition, biologic products, blood products, and more.
Some of the leading conditions treated with IV therapy are:
- Cancer
- Infectious Diseases
- Dehydration and Nutritional Support
- Autoimmune Disorders (e.g. rheumatoid arthritis, lupus, multiple sclerosis, etc.)
- Pain Management (e.g. fibromyalgia, migraines, etc.)
- Gastrointestinal Conditions (e.g. Crohn’s disease, ulcerative colitis, diverticulitis, etc.)
- Neurological Conditions [e.g. Alzheimer’s disease, myasthenia gravis, chronic inflammatory demyelinating polyneuropathy (CIDP), etc.]
- Respiratory Conditions [e.g. chronic obstructive pulmonary disease (COPD), severe asthma, emphysema, etc.]
- Hematological Disorders (e.g. hemophilia, anemia, etc.)
Benefits of Infusion
Infusion therapy offers unique benefits that other medication administration methods may not. In addition to IV therapy being offered in various settings (such as hospitals, in the patient’s home, in doctors’ offices, and in independent suites and ambulatory centers), infusion administration has improved efficiency of treatment, medication efficacy, and consistency. It also enhances the ability to manage long-term treatments and can be a cost-effective alternative to other methods.
Efficiency
Unlike oral-based treatments that require medications to pass through the digestive system, intravenous treatments streamline administration by introducing the products directly into the bloodstream. Especially in time-sensitive or emergency situations, efficient administration and induction of products can be crucial.
Treatment Efficacy
Even in cases that don’t rely on the speed of administration that infusions can provide, IV therapy can be useful in delivering potent medications that are not absorbed well via other methods. For instance, vancomycin is an antibiotic medication used to treat infections. While it can be taken orally, it has “poor bioavailability” and is primarily prescribed using the intravenous route.
Long-Term Management
 As previously mentioned, there are many different health conditions treated using infusion therapy. For some, these conditions are temporary, or only require temporary infusions. However, some disorders are not curable or require long-term treatment plans to manage symptoms. With IV therapy, patients have the ability to receive their treatments in their home, in a physician’s office, or at a nearby center, allowing them more flexibility in managing their therapy and any long-term implications.
As previously mentioned, there are many different health conditions treated using infusion therapy. For some, these conditions are temporary, or only require temporary infusions. However, some disorders are not curable or require long-term treatment plans to manage symptoms. With IV therapy, patients have the ability to receive their treatments in their home, in a physician’s office, or at a nearby center, allowing them more flexibility in managing their therapy and any long-term implications.
Cost-Effective
Similarly, site of care also has an impact on how much a treatment costs. With the options available to infusion patients, IV therapy is often a much more cost-effective alternative to hospital care.
Treatment Consistency & Control
Administering products via the intravenous route offers clinicians the unique opportunity to control the concentration of a solution, rate of infusion, and frequency of treatment. While many oral medications are offered in generic milligram amounts, infusions are often personalized based on patient weight to calculate the safest and most effective concentration and infusion rate.
Risks of Infusion
However, like with all medical treatments, IV therapy comes with its own risks. But by following strict practices, having educated clinicians, and carefully monitoring patients, these risks can be avoided in many situations.
Medication Side Effects
Many medications have side effects that clinicians and patients should be aware of before prescribing and accepting treatment. While some patients may experience side effects, others may not experience any. It is crucial that clinicians monitor patients during and after treatment to ensure that any side effects are noted, adverse reactions avoided, and treatments adjusted for the patient’s safety.
Infections
Because IV therapy is an invasive procedure (it involves puncturing the skin and entering the vein), there is the risk of infection. However, this can be minimized if clinicians follow strict best practices, maintain sterile conditions and materials, and monitor the injection site for signs of infection or irritation.
Allergic Reactions
It goes without saying that if a patient has an allergy to a specific product, they should not be administered said product. Unfortunately, some patients may be unaware of an allergy or could develop an allergy during administration. The severity of reactions can vary from irritation to anaphylaxis, so clinicians should always maintain the necessary equipment and medications nearby in the case of an emergency.
Hypervolemia
In some instances, hypervolemia could occur. Hypervolemia is an overload of fluid in the body that can lead to swelling, shortness of breath, and heart problems. To minimize this risk, clinicians should be sure to calculate appropriate infusion rates and amounts, and should monitor patients for signs of hypervolemia.
While IV therapy has risks like any other route of medication administration, these risks can be mitigated through education of both clinicians and patients, proper management of infusion materials and solutions, and careful observation.
Methods for Administering IV Treatments
There are two main methods of IV administration that should be considered when infusing. Depending on the product being administered and the patient’s details, both methods are effective in their own regard.
 IV Push
IV Push
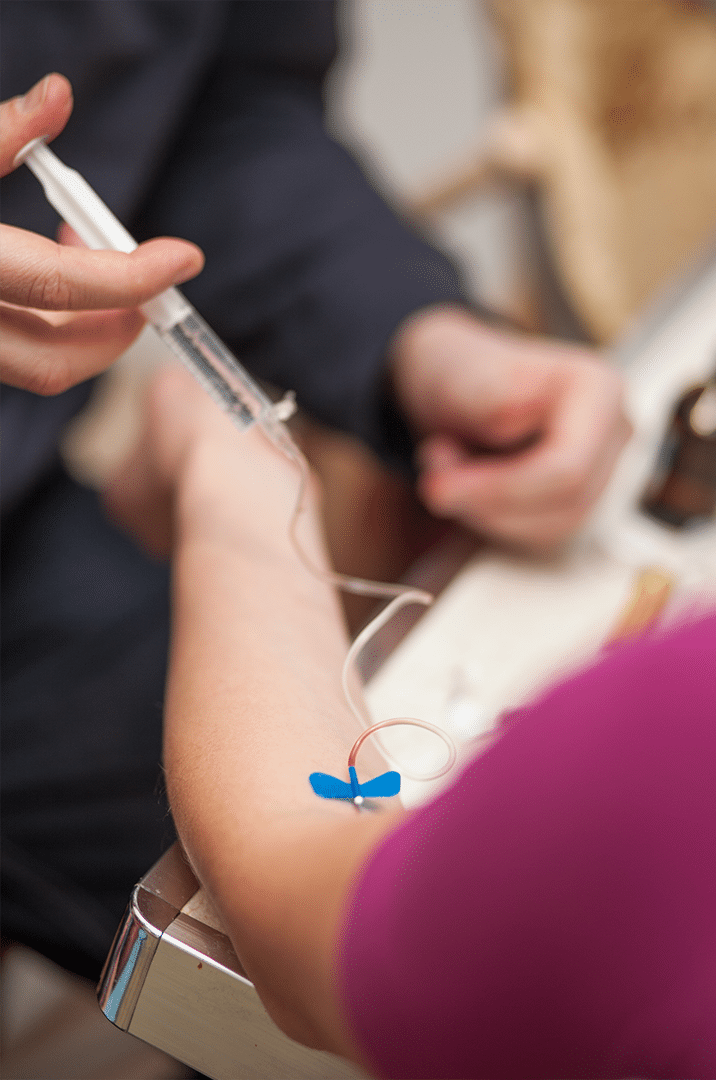
An IV push, or direct IV injection, is the administration of a small amount of product in a small amount of time. This method is ideal for instances when the effects of a medication are needed instantly, such as injecting epinephrine during cardiac arrest. In a situation that requires administration to be slow or in a large volume, a direct IV injection would not be the best method, but rather, an intravenous infusion.
Intravenous Infusion
 An intravenous infusion can be administered over a longer period of time and is used with high volumes of fluid. This method has more flexibility with administration time, allowing for intermittent or continuous infusion. For example, a solution of potassium chloride would be administered using the intravenous infusion method so as not to result in sudden increases of potassium in the blood, which can lead to heart problems.
An intravenous infusion can be administered over a longer period of time and is used with high volumes of fluid. This method has more flexibility with administration time, allowing for intermittent or continuous infusion. For example, a solution of potassium chloride would be administered using the intravenous infusion method so as not to result in sudden increases of potassium in the blood, which can lead to heart problems.
Both of these methods use different vascular access devices to aid in administration, and each device has its own purpose, reasons for use, and benefits.
What are vascular access devices?
Vascular access devices (VADs) are medical devices used to access a patient’s blood vessels. They can be used to infuse medications, fluids, and nutrition; transfuse blood products; draw blood samples; and for invasive monitoring of hemodynamics.
Types of Vascular Access Devices
There are many different types of vascular access devices, but some of the most common include peripheral intravenous catheters, central venous catheters, peripherally-inserted central catheters, and implanted ports.
While some vary more than others and each have their own pharmaceutical considerations, a primary difference between VADs is the length of time they can be left in place.
Peripheral Intravenous Catheters (PIVCs)
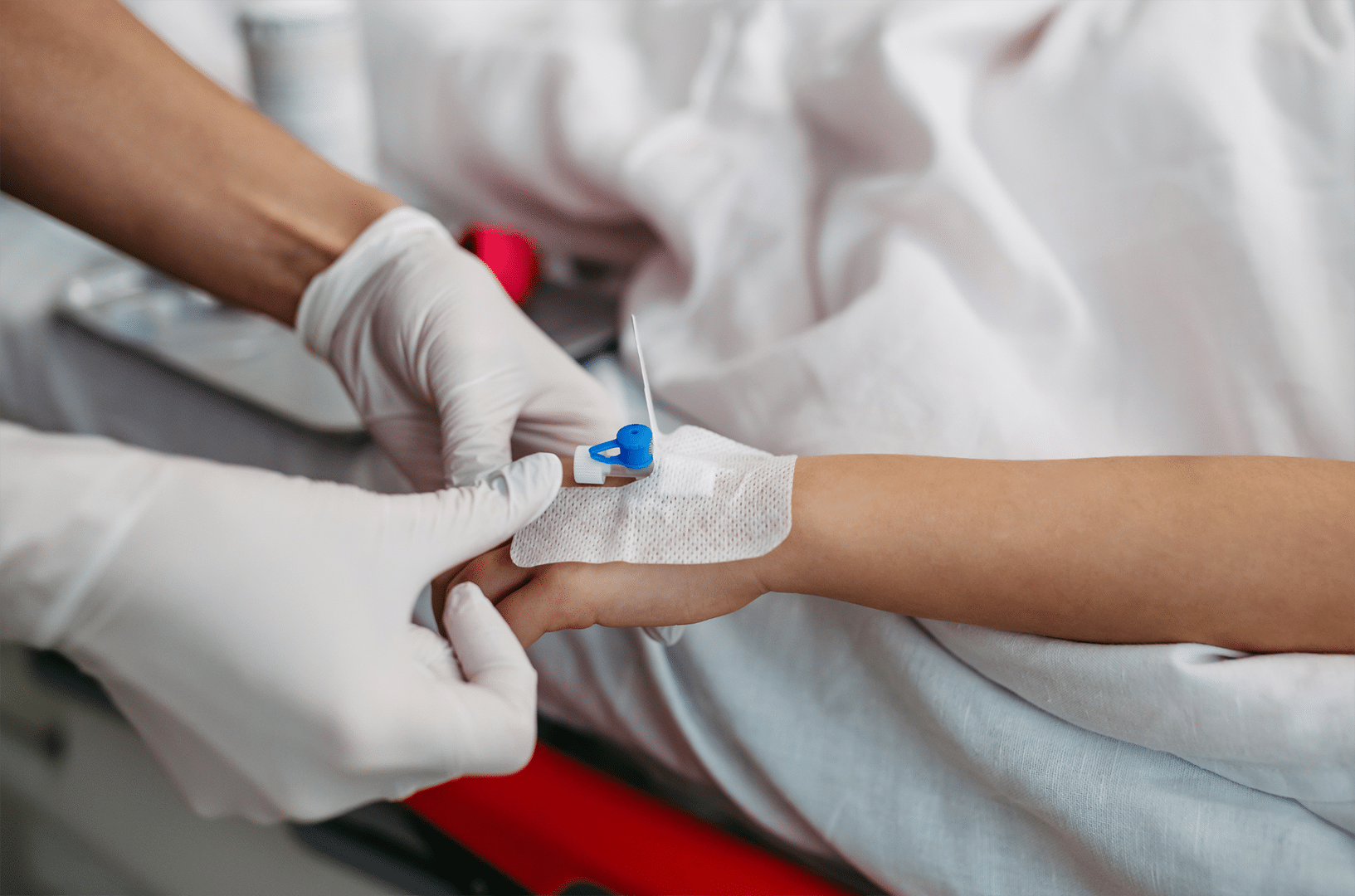 The most common VADs are peripheral intravenous catheters (PIVCs), or cannulas. These are short plastic tubes typically inserted into a vein in the arm or hand and are ideal for short-term use in inpatient or outpatient settings.
The most common VADs are peripheral intravenous catheters (PIVCs), or cannulas. These are short plastic tubes typically inserted into a vein in the arm or hand and are ideal for short-term use in inpatient or outpatient settings.
Pharmacist Considerations
Not all medications can be administered using PIVCs, so it is important to ensure medication compatibility, appropriate medication concentration, and other properties such as pH to minimize the risk of adverse reactions, such as infiltration and extravasation.
Central Venous Catheters (CVCs) and Tunneled Catheters
Central venous catheters (CVCs) are inserted into large veins (e.g. jugular or subclavian) in the neck, chest, or groin. Tunneled catheters are long, hollow plastic tubes inserted into large central veins in the neck or chest that are tunneled under the skin to secure placement.
These catheters are ideal for long-term use or for patients that require invasive monitoring. They are intended for patients requiring prolonged intravenous therapy or are in a critical care setting.
Pharmacist Considerations
Again, ensuring medication compatibility is key, as there may be multiple medications being administered through a single CVC. Clinicians should monitor for signs of infection, as these VADs are accessed frequently and are maintained for longer periods of time.
Peripherally-Inserted Central Catheters (PICCs) and Midline Catheters
Peripherally-inserted central catheters (PICCs) are inserted in a peripheral vein in the upper arm and threaded to a central vein. Midline catheters are very similar to PICCs, with the exception of the tube length; midlines are about half the length of PICCs.
These vascular access devices allow for long-term vascular access and are often used in patients needing extended courses of antibiotics or chemotherapy. They can be used in the outpatient setting or in outpatient infusion centers.
Pharmacist Considerations
For these catheters, it is important to assess the need for flushing protocols to maintain patency and reduce the risk of thrombosis. Clinicians should monitor for signs of infection, as these VADs are accessed frequently and are maintained for longer periods of time.
Implantable Ports
 An implantable port is a device placed under the skin of the chest that is connected to a catheter inserted in a central vein. It allows for repeated and intermittent access to central vasculature, and is ideal for patients requiring frequent intermittent intravenous treatments.
An implantable port is a device placed under the skin of the chest that is connected to a catheter inserted in a central vein. It allows for repeated and intermittent access to central vasculature, and is ideal for patients requiring frequent intermittent intravenous treatments.
Pharmacist Considerations
Clinicians should ensure proper medication administration techniques to avoid complications such as extravasation.
Vascular Access Device Management
Medication Administration Considerations
When managing patients with vascular access devices, several medication factors are important to consider:
- Compatibility: Always verify medication compatibility, especially when administering multiple medications through the same vascular access device.
- Infusion Rates: Adjust infusion rates based on the type of vascular access device and patient needs, particularly for those with fluid restrictions or for certain medications, such as potassium chloride.
- Medication-Specific Properties: Consider the osmolality, tonicity, and pH of the intravenous fluid or medication. The cytotoxic properties of a medication classified into non-cytotoxic, irritant, and vesicant refers to a fluid or medication’s direct effect on vasculature and the surrounding tissue. Knowledge of these properties help determine the most appropriate VAD to administer a medication or fluid through.
- Monitoring: Regularly monitor the insertion site for signs of infection, phlebitis, or infiltration. Prompt identification of these can prevent or minimize complications such as extravasation.
For all medication administration-related considerations, it is important to utilize your medication information resources for the most up-to-date information on specific medications.
RxToolKit
Software like RxToolKit is specially designed to provide up-to-date medication information for infusions, antibiotics, and injectables. With two products built into one solution, medication resource platform RxToolKit is maintained by clinicians to provide the crucial information needed for safe and effective administration.
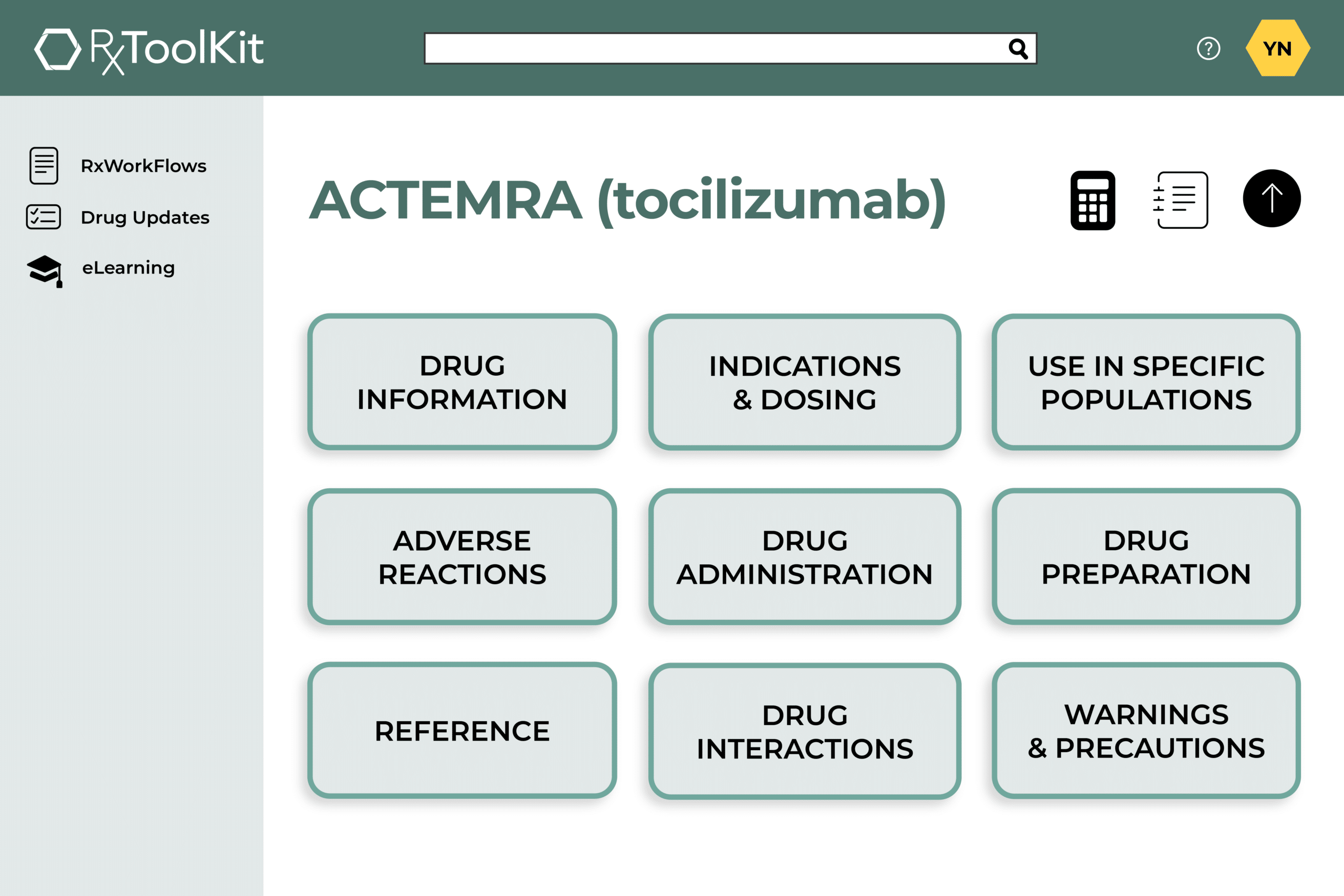 The first product included in the software, RxWorkFlow, is a library of over 300 medication guides for infusion and injectable products. Included in each guide are built-in calculators to help clinicians save time and ensure appropriate infusion rates based on the patient. Guides feature all of the critical information of package insert in the easily-accessible, comprehensive digital format. RxToolKit was founded by pharmacist Chuck DiTrapano, RPh, and is maintained by a team of clinicians to guarantee up-to-date information.
The first product included in the software, RxWorkFlow, is a library of over 300 medication guides for infusion and injectable products. Included in each guide are built-in calculators to help clinicians save time and ensure appropriate infusion rates based on the patient. Guides feature all of the critical information of package insert in the easily-accessible, comprehensive digital format. RxToolKit was founded by pharmacist Chuck DiTrapano, RPh, and is maintained by a team of clinicians to guarantee up-to-date information.
The second product in the software, RxELearning, offers clinicians medication-specific training courses to enhance comprehension. Through partnerships with organizations like the Infusion Nurses Society and the Immunoglobulin National Society, RxELearning also provides clinicians with a library of infusion and immunoglobulin-specific continuing education (CE) and continuing medical education (CME) units.
Using a solution like RxToolKit to ensure best practices, clinical comprehension, and up-to-date resources can minimize the risk of medical errors associated with expired medication guidelines, incorrect infusion rates and calculations, and overwhelming medication updates.
Complications Associated with VADs and Their Management
Similar to infusion therapy, vascular access devices come with potential complications that healthcare teams must be aware of.
Infections
One of the most significant risks associated with VADs is infection. Central line-associated bloodstream infections (CLABSI) can lead to patient morbidity and increased healthcare costs. Management includes initiation of broad-spectrum antibiotics to cover bloodstream infections and source. This can be controlled with removal of the VAD, if possible.
Thrombosis
Thrombosis, the formation of blood clots, can occur within the catheter or the surrounding veins. This can lead to deep vein thrombosis or catheter occlusion. Management includes the initiation of therapeutic anticoagulation and removal of the VAD with catheter occlusion.
Extravasation
Extravasation occurs when IV fluids or medications leak into the surrounding tissue, potentially causing pain and tissue damage. Irritant or vesicant fluids or medications can increase this risk. In the case of extravasation, clinicians should utilize medication information resources for management of specific medications. Management can include application of cold or warm compresses and the administration of medication-specific antidotes (e.g. hyaluronidase, phentolamine, etc.).
The Pharmacist’s Role in VAD Management
Pharmacists have a unique and key role in the infusion process and the management of vascular access devices. Their involvement can significantly enhance patient safety:
- Medication Management: Assessing the appropriateness of medications administered through VADs, ensuring accurate dosing of medications, and compatibility of multiple medications being administered through a single line.
- Patient Education: Providing education on the importance of adherence to prescribed therapies and VAD care techniques.
- Monitoring: Participating in patient monitoring, assessing for signs of complications, and recommending interventions when necessary.
- Policy Development: Contributing to the development of institutional policies regarding VAD use, maintenance, and infection control practices.
Infusion therapy is a crucial method used in the treatment of many conditions that affect patients. Understanding how to use the vascular access devices needed for infusion therapy as well as the benefits and risks associated with them is key to providing effective treatment and better patient outcomes.
Pharmacist involvement in the management of these devices is fundamental to ensuring safe medication administration, enhancing patient care, and promoting patient safety.