Bailey Klingaman explores the definitions of infusion nurses and pharmacists, the responsibilities that come with their titles, and how to enter the professions. Thank you to Pamela Jones McIntyre, MSN, RN, CRNI, OCN, Ig-CN, VA-BC and Chuck DiTrapano, RPh for their contributions on why to enter the field and pursue a career as an infusion nurse or pharmacist.
Picture an infusion treatment happening in your head. Who do you see?
No matter whether the infusion is happening in a hospital, a clinic, or in the patient’s home, you probably see two people: the nurse and the patient. Both are integral to the infusion process. I mean, how do you administer an infusion with no one to actually administer it, or how do you infuse someone without someone to infuse?
But there are actually many moving parts that contribute to a single infusion treatment: the medication supplier, the hospital/clinic manager, the wonderful administrator at the front desk, and so many others. All of these people play an important role in ensuring a patient has a safe and comfortable therapy session.
Today, I want to talk specifically about the two (or three) clinical roles that are directly involved in an infusion, what their responsibilities really are, and how they earned their titles of infusion nurse, pharmacist, and pharmacy technician.
What is an infusion nurse?
An infusion nurse is a nurse who specializes in the administration of intravenous treatments. The infusion nurse plays a vital role in the care of patients with chronic diseases, cancer, dehydration, and other conditions that may require alternative methods of administration, quick delivery, or controlled dosing.
Where are infusion nurses needed?
The most obvious setting that administers infusions is likely one that everyone has experienced at one point or another: the hospital setting. While the hospital is what might come to mind first – along with the mental image of people in hospital gowns walking around with their nutrient infusion – there are quite a few other settings where infusions take place, including:

- Ambulatory infusion centers
- A physician’s office
- Your home
It is also likely that when you think of an infusion treatment, you think of a chemotherapy or a nutrition/hydration infusion. However, intravenous treatment is not limited to oncology and nutrition, and can extend to blood transfusions, antibiotics, and specialty biologics.
Specialty biologics treat various disease states across many specialties, including, but not limited to:
- Allergy & Immunology
- Gastroenterology
- Neurology
- Rheumatology
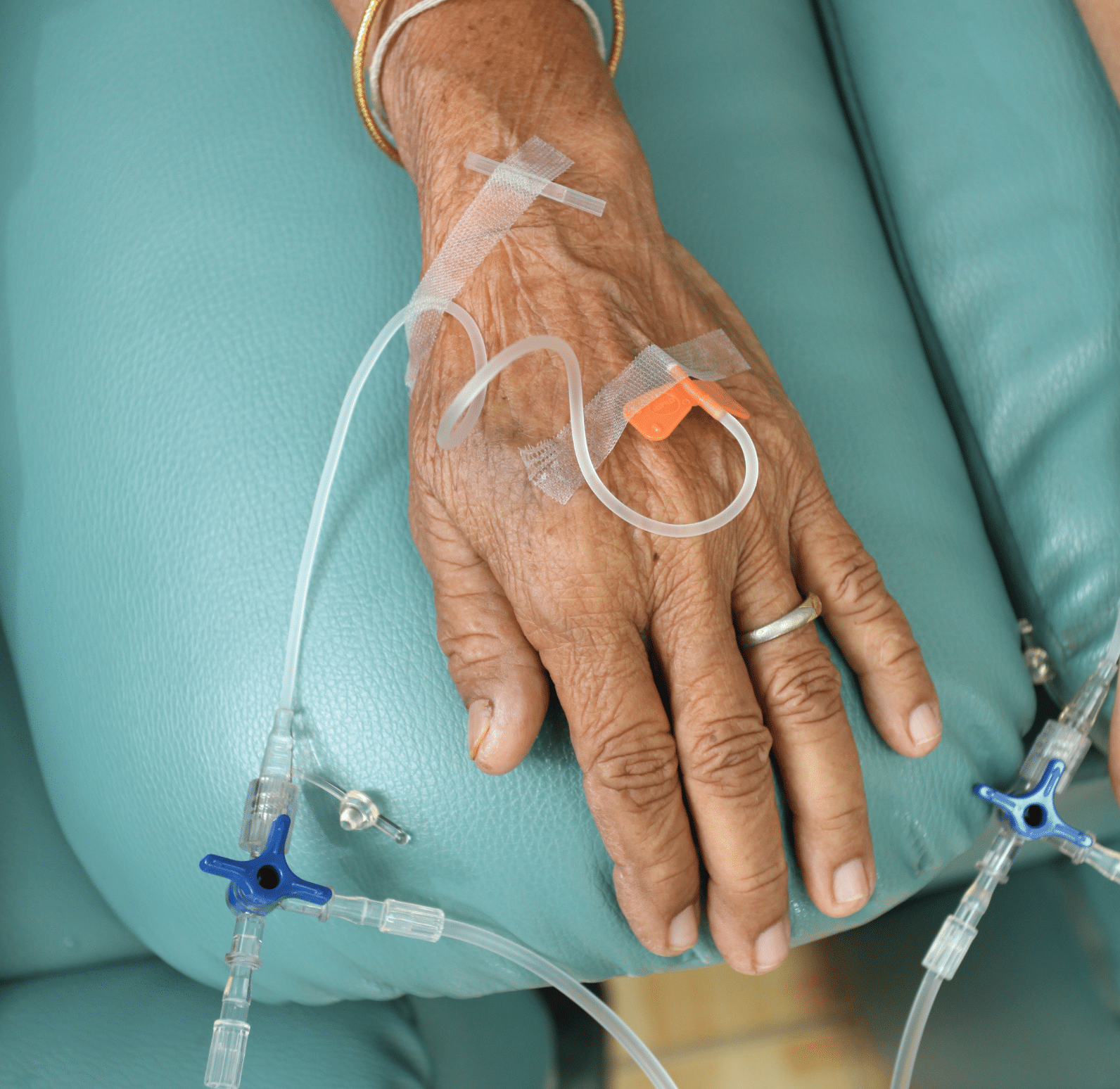
There are also different methods of vascular access that an infusion nurse may use, as the frequency, comfortability, and medication may impact the patient’s treatment. Depending on the conditions of therapy, an infusion nurse may administer the medication through a peripheral IV, a midline catheter insertion, a central IV line, a peripherally inserted central catheter (PICC), an arterial line, or a venous access port.
What are the responsibilities of an infusion nurse?
Along with placing the infusion access point, infusion nurses have an array of responsibilities that impact their workplace, fellow clinicians, and patients. In addition to starting lines, an infusion nurse’s duties can include:
- Training new nurses on initiating and maintaining IV access
- Administering medications and fluid treatments
- Troubleshooting challenges or unforeseen complications
- Collaborating and communicating with other clinicians
- Educating the patient and/or family on the treatment
- Medication
- The prescribed treatment plan
- Potential side effects
- Possible adverse events
- Treatment
- The access point
- The tubing
- The catheter maintenance and management
- Reviewing lab results
- Care
- Dressing changes for PICCs, midlines, and central lines
- Preventing infections and assessing patency
- Monitoring the response to treatment
- Discharging patients
- After-care instructions
- Medication
What is required to become an infusion nurse?
Given the complexity of intravenous therapy, infusion nurses must earn either an Associate Degree in Nursing or a Bachelor of Science in Nursing in order to become licensed. After obtaining a degree, they are required to complete an accredited nursing program and obtain a nursing license to become a registered nurse (RN).
As an RN, they can legally administer infusions until it is time to renew their license. Each state has different requirements for license renewal, but nurses will generally need to submit an application, complete the required number of continuing education hours, and pay a small fee.
If an RN wishes to obtain further credentials, they can choose to become certified by the Infusion Nurses Society (INS).
How do I become a certified infusion nurse?
To become a nationally recognized Certified Registered Nurse Infusion (CRNI®), the RN must have at least 1600 hours of experience in infusion therapy in the last two years in order to apply for the CRNI® exam. This exam includes questions on the Principles of Practice, Access Devices, and Infusion Therapies. Once the exam has been passed, the RN will receive CRNI® credentials for the next three years until renewal is required.
To renew recertification, certified infusion nurses can either pass the CRNI® exam again or complete 40 recertification units. Of these 40 RUs, INS requires a minimum of 30 to be earned through INS continuing education meetings. According to INS, for the remaining 10 units, nurses may:
- Participate in an INS Learning Center webinar
- Complete the Journal of Infusion Nursing CE Test
- Publish a manuscript in the Journal of Infusion Nursing
- Serve as an Editorial Reviewer for the Journal of Infusion Nursing
- Publish an infusion-related manuscript in a peer-reviewed journal
- Publish a chapter or edit an infusion-related book
- Attend INS local chapter education programs
- Teach infusion therapy-related education programs
- Attend a non-INS education meeting (from a sponsoring organization)
Why become an infusion nurse?
By Pamela Jones McIntyre, MSN, RN, CRNI, OCN, Ig-CN, VA-BC
From what I have learned from my colleagues, becoming an infusion nurse was not on their radar as nursing students. This is especially true for many of us, considering the specialty didn’t exist. Other niches such as orthopedics, pediatrics, and obstetrics were favorites, but the option of ‘infusion’ as a nursing domain wasn’t available. I routinely glean program curriculums for a course in ‘Infusion Nursing’ without satisfaction.
Considering there is no corner of the discipline that is not touched by infusion, how does someone decide to become an infusion nurse, and from where will these experts evolve?
Most of the infusion specialists I have run across have become fascinated by the craft after experiencing the acute nature and intricacies of the practice. We learned that minute interventions could lead to drastic results, and sought to improve those outcomes through our study and dedication.
There has never been a more exciting time to join this progressive club. The innovations, discoveries, and developments in disease management by infusion therapy have been nothing short of amazing. Despite these advances, the acuity of our patients is such that the discernment of human touch will always be necessary for the care of the patient population served by infusion nurses. All you need to do is pick up a magazine or access the internet and you will be immersed in advertisements for the newest biologic therapy to treat serious, chronic, and previously untreatable diseases.
Infusion of these therapies requires a remarkable amount of knowledge, skill, intuition, and emotional intelligence. The need for these experts grows exponentially with each new drug’s approval. Perhaps someone in your circle is having their life improved or extended by infusion therapy this very day.
The specialty of infusion nursing is in critical demand today and that shortfall will only increase tomorrow. Whether it is cancer, immune disorders, or one of the myriad conditions treated by this group of professionals, infusion nurses have the potential to change lives on a daily basis. Come join us!
What is a pharmacist?

A pharmacist is a medication expert who dispenses prescriptions and specializes in the proper use and administration of medications. Depending on the provider, a pharmacist might also conduct health and wellness screenings, provide advice on leading a healthy lifestyle, and offer immunizations. There are different kinds of pharmacists with varying responsibilities and environments, including:
- Community pharmacists
- A community pharmacist works in retail pharmacies, which can include an independent pharmacy, a specialty pharmacy, a large-scale chain store, and more. In these settings, the pharmacist is there to provide the community with their medications, answer any questions they may have, and ensure the safe dispensing of these drugs.
- Pharmaceutical pharmacists
- A pharmacist in the pharmaceutical industry works in sales, marketing, research, or development fields of medication production. It is their duty to develop drugs, conduct clinical trials, create guidelines for safety, and monitor medication quality.
- Clinical pharmacists
- A clinical pharmacist works in a healthcare setting such as a hospital or clinic, and is more directly involved with patient care. A clinical pharmacist is less likely to spend time filling prescriptions, and more likely to work with patients and other clinicians in the preparation and administration process.
- Nuclear pharmacists
- A nuclear pharmacist works with radioactive drugs and radiopharmaceuticals for nuclear medicine testing and imaging. They are responsible for ensuring the safety of radioactive drugs in diagnosing and treating certain conditions.
What is the role of a pharmacist in infusion?
A pharmacist who works with patients receiving infusions (i.e. an infusion pharmacist) is likely to be classified as clinical, although they may also be considered a community pharmacist as well. The infusion pharmacist is responsible for accurately preparing (and sometimes administering) the medication and monitoring the patient throughout the treatment. They can also be a resource for patients regarding their condition and treatment plan.
While an infusion pharmacist’s responsibilities can differ depending on setting and circumstances, their duties can generally include:
- Preparing infusion medications and solutions according to protocol and best practices
- Administering medications according to the treatment plan
- Monitoring patient reactions to the treatment
- Identifying potential drug interactions and precautions that should be taken
- Making adjustments to the treatment if necessary
- Educating patients and/or family on the condition, the treatment plan, and the potential side effects, and answering any questions they might have
- Maintaining a drug and supply inventory and ordering replenishments when necessary
- Evaluating new drugs for safety and effectiveness
- Proposing changes to drugs and treatments based on medication updates
What is required to become a pharmacist?
Prior to 2006, pharmacists needed to earn a Bachelor of Science in Pharmacy and pass the licensure exam to practice as a registered pharmacist (RPh). Today, aspiring pharmacists must complete a pharmacy program recognized by the Accreditation Council for Pharmacy Education (ACPE).
Some of these programs require a Bachelor degree, others require a minimum of two years of undergraduate education, and some require applicants to take the Pharmacy College Admissions Test (PCAT).Once the student completes the program, they have obtained their Doctor of Pharmacy degree, but infusion pharmacists are required by law to be licensed in their state of practice.
States have different processes to achieve licensure, but candidates are generally expected to pass the North American Pharmacy Licensing Exam (NAPLEX) and either the Multistate Pharmacy Jurisprudence Licensure Exam (MPJE) or a state-specific pharmacy law exam. Some states require candidates to complete a six-month clinical internship in addition to taking these exams.
What further education can pharmacists receive?
After earning their PharmD and becoming a licensed RPh, pharmacists may be required or choose to pursue additional certifications. For example, in order to administer vaccines, a pharmacist has to be certified through the American Pharmacist Association’s Pharmacy-Based Immunization Delivery program.
Regardless of additional certifications, pharmacists are expected to take continuing education courses throughout their careers to stay up-to-date on new practices and advances in the field.
What is the role of a pharmacy technician in infusion?

In addition to pharmacists, the pharmacy technician also plays an important role in infusion therapy. As a supporting role to a pharmacist in supplying prescriptions and medications to patients, and under the supervision of a pharmacist, pharmacy technicians also:
- Prepare intravenous solutions and medications
- Calculate the amounts and mix each ingredient to create the proper solution
- Manage and maintain medical supply areas
- Supervise other pharmacy staff
- Provide information regarding medication to patients or other clinical staff
What is required to become a pharmacy technician?
Regardless of state, aspiring pharmacy technicians must have a high-school diploma or equivalent and have no record of felony or drug-related crimes. However, as of September 2023, all states except Delaware, Hawaii, New York, and Pennsylvania require technicians to be registered or licensed.
In order to gain licensure, most states require the technician to register with the state’s Board of Pharmacy, and some require additional training program completion or certification. It may be possible for a technician to obtain an entry-level job and gain experience in the field, but they will likely not be granted the full duties of their position without certification.
How do I become a certified pharmacy technician?
Again, the requirements for certification vary by state. However, it is common for a state to require national certification by the Pharmacy Technician Certification Board (PTCB). To obtain this certification (CPhT), the technician must pass the Pharmacy Technician Certification Exam (PTCE), which includes testing on Medications, Federal Requirements, Patient Safety & Quality Assurance, and Order Entry & Processing. One of the ways technicians can study for this exam is by purchasing virtual courses by Pharmacy Technician University.
PTCB CPhTs must renew their certification every two years by completing a minimum of 20 hours of continuing education and paying a small reinstallment fee.
Why become a pharmacist/pharmacy technician?
By Chuck DiTrapano, RPh

I didn’t find pharmacy…pharmacy found me.
My journey to becoming a pharmacist started with the decisions I made after high school about my future. When my parents and I were discussing what to do after graduation, we looked to respected members of the community for inspiration.
There was our community pharmacist, Joe Klein of Klein Pharmacy. Joe was a good and kind man who often assisted my family with healthcare questions. He had become our family’s pharmacist and gained our trust and confidence quickly. He was the kind of man that was respected in our community and had a fulfilling career; the kind of career my parents and I were looking for.
Through his mentorship and guidance, I applied and was accepted to the Albany College of Pharmacy. After beginning my formal education in pharmacy, I realized early on that it offered amazing and diversified opportunities. I was introduced to retail pharmacy, hospital pharmacy, research, and long-term care pharmacy. Each practice setting offered its own set of challenges, and I knew that I would never be bored.
As a pharmacist, I was able to help people. Pharmacists were the most accessible health care professionals to the public, as there was no appointment necessary. They possessed knowledge about something that almost everyone needed: medicine. From over-the-counter to prescription medication for serious illnesses, the knowledge of a pharmacist is relevant to everyone.
I find that the profession continues to challenge me. There are always new medications to learn and treatments to evolve. Pharmacy is not a stagnant industry, and as more and more ways of providing care are introduced, the importance of the job grows as well. I have grown to love the profession, and hope you will too.