Bailey Klingaman walks through the technology available to infusion teams that relieve burdens on clinicians and reduce medication errors. From smart IV pumps to the new Smarthood™, explore the technology and its implications for patient safety.
Intravenous (IV) infusion therapy is a complex delivery method involving the administration of medications or fluids directly in the vein. While there are many benefits to infusion delivery, including clinical control of the speed at which medication is administered and its effectiveness in treating a variety of chronic health conditions, infusion therapy has its own risks.
Studies have shown that infusions are associated with 54% of all adverse drug events, 56% of medication errors, and 61% of serious and life-threatening events. Infusion medications are also twice as likely to be involved in harmful errors than medications with other delivery methods.
The most common causes for medication errors are system failures, such as miscommunications, lack of standardized procedures, and mistakes in tracking medication orders. By embracing technological solutions—smart infusion pumps, barcode scanners, vein-finder technology, and more—and decreasing the opportunity for human error, we can improve safety and reduce preventable medication harm for patients and clinicians.
Smart Infusion Pumps
An external infusion pump is a device used to deliver medication and fluids into a patient’s body. Pumps can be designed to deliver in large or small amounts, and can be stationary or ambulatory (portable or wearable). You can learn more about the different kinds of infusion pumps in our article, “Intro to Administration Methods & Infusion Devices”.
 Smart pumps are advanced infusion pump devices that are equipped with safety features. They can be programmed to include predetermined clinical guidelines, dose error reduction systems (DERS), and medication libraries. When administering an infusion, the smart pump is designed to alert the user of any risks, including adverse events, inappropriate parameters, clinical notices, soft stops, and hard stops.
Smart pumps are advanced infusion pump devices that are equipped with safety features. They can be programmed to include predetermined clinical guidelines, dose error reduction systems (DERS), and medication libraries. When administering an infusion, the smart pump is designed to alert the user of any risks, including adverse events, inappropriate parameters, clinical notices, soft stops, and hard stops.
The prevalence of smart pumps in healthcare has increased drastically. In 2007, the American Society of Health-System Pharmacists (ASHP) found that 44% of all hospitals in the United States were utilizing smart pumps. In 2013, that number had increased to 72.9%, and in 2018, 89.5% of hospitals had smart pumps.
But smart infusion pumps aren’t just helpful for hospitals. The Institute for Safe Medication Practices (ISMP) also encourages the use of smart pumps as a strategy to improve safety and reduce the frequency and severity of errors.
Benefits of Smart IV Pumps
Studies have found that smart infusion pump technology can have a drastic impact on error reduction and prevention, especially for errors linked to incorrect dosing, rates, and pump failure.
A recent study determined that the implementation of smart pumps in correlation with a medication library and DERS prevented 1,136 errors and could avoid 300 adverse events in an adult intensive care unit (ICU) in a two year period. The researchers found “a 70% reduction in reporting errors related to basic drug infusions,” and “an 80% reduction in infusion-related drug errors.”
Another study analyzed the implementation of smart pumps with patient-controlled analgesia (PCA) and found a reduction in adverse events of 0.18 for every 100 pumps a day.
In combination with medication libraries and DERS, evidence has shown the positive impact smart infusion pumps can have on patient safety, particularly when used in places of service with a high volume of patients.
Challenges
However, while smart pumps are innovative devices and have been increasingly adopted in healthcare settings, user errors, insufficient usage, and incorrect programming can still occur and have impacts on safety results. In addition, the reliance of smart infusion pumps on integration with DERS and medication libraries makes the case for the pump alone difficult.
An Australian study found that while smart pumps decreased the number of infusions with errors from 76 to 25, the addition of medication error-prevention software only resulted in 6 infusions with errors, an almost 80% decrease in errors.
Furthermore, the integration of drug libraries with smart pumps takes time and requires further updates to maintain timely compliance. For wireless systems, library update delays can impact administration guidelines and can take up to 192 days after drug updates for the library to become compliant. And in cases of library connection to the smart pump, the ability to neglect or bypass the library can have negative impacts on pump effectiveness.
Some smart pump users have also experienced an over abundance of alerts, leading to alert fatigue and frequent overrides. One study discovered that over 75% of alerts from smart pumps were bypassed in 15 observed hospitals. The bypassed alerts did not have an impact on improving error reporting rates, as they did not have the intended effect on the medication administration.
Ways to Improve
It’s no secret that while smart pumps are a perfect solution on paper, their implementation can be difficult to manage. But with maintenance and preparation, they have the potential to greatly improve patient safety.
Teaching library compliance is critical, as non-compliance can have negative effects on the application of smart pumps. While a study showed that pharmacists and nurses complied with the drug library 100% of the time across six ICUs, it also recognized that they were most familiar with the drug library, what it included, and what medications were not programmed in. In comparison, other departments were found to bypass the medication library 34% of the time due to extreme restrictions and high alert counts.
To help ease the fatigue from alerts, the smart pump was altered to reduce non-compliance and still maintain safe administration guidelines. Over three months of applying recommendations and adjustments to the infusion pumps, specifically reducing the amount of soft alerts, alert frequency decreased from 4% to 1.16%, reducing the correlating overrides by 55%.
Another programming adjustment that had positive effects on error reduction was encouraging the smart pump to make dose corrections due to under- or over-dosing. For heparin infusions, the smart pump made 13 dosing corrections, preventing harm to the patients and saving the hospital $113,750.
Barcode Medication Administration Technology
Barcode scanners are optical readers, meaning they read visual information and translate it into digital information, which read and decode data from barcodes. There are many different kinds of barcode scanners classified by the type of technology they use to scan the barcode, including:
- Laser Scanner – uses a laser to emit light and reads the light reflected back from the barcode
- LED Scanner – hundreds of tiny LED lights measure the ambient light emitted from the barcode itself
- Camera-Based Scanner – uses a camera to take an image of a barcode, which is then scanned and decoded

Barcodes can also be linear (1D), two-dimensional (2D), or composite (a combination of 1D and 2D). Linear barcodes are most common, and can be found on medications in the form of a 10-digit National Drug Code (NDC), which identifies the manufacturer, product, and package size. On the other hand, two-dimensional barcodes can include more information, such as lot number and expiration date. You can learn more about the kinds of barcodes in the WeInfuse article, “What’s in a Barcode? Understanding DSCSA and Leveraging Barcodes in Your Operation Today” by Bryan Johnson.
Barcode implementation in healthcare has been a lengthy process. When the first barcode technology was developed in the 1990s, the ASHP found that only 1.1% of hospitals were actually using the tech in 1999. A re-survey in 2002 found that still, only 1.5% of hospitals were utilizing barcodes in medication administration. However, a 2018 report by The Leapfrog Group found that of 2,000 surveyed hospitals, 98.7% were utilizing barcode technology—although, only 34.5% were using the technology effectively.
Benefits of Barcode Technology
When used effectively, barcode medication administration technology (BCMA) can prevent medication errors and improve patient safety. By verifying the necessary information for both the patient and the medication, BCMA confirms the “five rights” of medication administration: right patient, right medication, right dose, right route, and right time.
Barcode technology can be extremely effective when used with electronic health records (EHRs). They can be used at many points in the medication delivery system, from ordering medications and managing inventory to keeping track of patient information. When integrated with EHRs, the BCMA is able to confirm the five rights by scanning patient-specific barcodes and medication barcodes, double checking appropriate treatment and improving safety.
Barcode technology also works with electronic medication administration records (eMARs). These can be used in conjunction to eliminate dispensing, transcription, or administration errors at the point of care.
Challenges
However, while nurses seem to favor BCMA and eMAR technology to previous medication administration systems, studies found that its implementation did little to reduce the time spent on administration. Further research must be conducted to determine the effectiveness of this technology on reducing clinical burdens.
Studies have also shown that while barcode technology has become much more widely adopted in healthcare, its implementation is complex. Increased workload and disrupted processes have led to workarounds that interfere with the intended impact of the technology, such as carrying pre-scanned medications. These workarounds can lead to errors and counteract the reason for the technology.
Ways to Improve
Radio frequency identification (RFID) is a potential replacement for current barcode technology, particularly in inventory management. While barcode scanners require a line of sight to scan one code at a time, RFID scanners have the ability to scan multiple codes at a time. This is particularly helpful when scanning a high volume of items.
The most likely points of use for RFID technology are in blood products and IV bags, as their containers are typically difficult to place labels on and require a large amount of information to be included.
However, while RFID technology can be a more efficient solution than traditional barcodes, it is also much more expensive. Users looking to implement some kind of scanning technology for their operations should weigh the benefits between traditional BCMA and RFID to determine the best possible option for their practice.
Vein-Finder Technology
 Vein finders are devices that use technology to help healthcare providers locate veins. They are most helpful in use with patients with difficult venous access—which can be due to obesity, dark skin, history of intravenous drug use, or other causes. For these patients, infusions and venipuncture can be painful and complicated. Vein finders help eliminate the repeated and incorrect insertion of catheters by displaying the location of the veins, aiding in insertion accuracy.
Vein finders are devices that use technology to help healthcare providers locate veins. They are most helpful in use with patients with difficult venous access—which can be due to obesity, dark skin, history of intravenous drug use, or other causes. For these patients, infusions and venipuncture can be painful and complicated. Vein finders help eliminate the repeated and incorrect insertion of catheters by displaying the location of the veins, aiding in insertion accuracy.
The different types of vein finders have their own features and benefits. The most common types of vein finders include:
- Handheld Vein Finders — portable devices used in emergency or outpatient settings for quick venous access
- Tabletop Vein Finders — large and powerful vein finder devices used in hospitals or clinical settings for detailed images of veins (best for complex procedures)
- Wearable Vein Finders — portable devices worn on the healthcare provider’s arm or head to allow for hands-free operation
Vein finders can also utilize different kinds of technology: near infrared (NIR), ultrasound, and transillumination. NIR technology is found in vein finders most often, and works by shining a bright light on the skin. The hemoglobin in the patient’s vein absorbs the light and projects a map of the veins on the skin.
Benefits of Vein Finders
The primary benefit of vein finder technology is improving the comfort for the patient, as making multiple attempts to find a vein can be painful or lead to infections and complications. Vein finder technology can also improve the accuracy and efficiency of vein location for healthcare providers by identifying vein location, size, and trajectory.
Vein finders are a non-invasive solution to vein location and can eliminate the need for traditional techniques like palpation (the clinician using their hands to feel around the body) or tourniquet usage. Particularly for patients receiving frequent IV infusions, blood transfusions, or injections, vein finders can significantly alleviate anxiety, discomfort, and the possibility for complications.
Challenges
While NIR technology has its benefits, it also has challenges. The projection of the veins on the skin can make it difficult for clinicians to determine the depth of the vein, and depending on the specific type of vein finder being used, may require additional hands to both work the vein finder and complete the insertion.
Ways to Improve
Clinicians may prefer to use one of the other two kinds of vein finder technology—ultrasound or transillumination—if NIR technology is not the correct fit.
Ultrasound technology uses soundwaves and the reflections sent back from contact with the veins to generate an accurate image of the venous structures. This allows for deeper mapping, but for that reason is primarily used for veins six millimeters or deeper under the skin. Ultrasound technology requires significantly more training than NIR technology.
Another option is transillumination technology, which produces bright LEDs that are absorbed by the blood in the veins. This not only produces an accurate depiction of the layout of the veins, but can also portray the size and depth of the vein. This option can view deeper into the skin than traditional NIR technology, and is considered more cost effective.
Smart IV Hoods – IVWMS Tech
Smart IV hoods are a revolutionary new technology based on laminar flow hoods, or clean benches. Laminar flow hoods are enclosed workstations used to maintain sterile environments. Traditional hoods use filters to remove airborne contaminants from the environment and ensure sterile medication preparation.
 A new product, Smarthood™, by Germfree is modelled after traditional laminar flow hoods, but includes key features to make IV infusion preparation as safe, sterile, and standardized as possible.
A new product, Smarthood™, by Germfree is modelled after traditional laminar flow hoods, but includes key features to make IV infusion preparation as safe, sterile, and standardized as possible.
Smarthood™ is an “IV Workflow Management Solution” (IVWMS) designed to help automate the verification, tracking, and documentation of compounded sterile preparations (CSPs). According to a Pharmacy Practice News article, IVWMS technology has five key attributes:
- Uses machine-readable coding (barcodes, RFID, etc.) to verify products during the compounding process with appropriate hard stops
- The ability to automatically perform calculations and conversions
- Step-by-step guidance for compounding, including documentation of all steps and components
- Uses videos or pictures for volumetric verification and scales for gravimetric measuring
- The ability to work with EHRs to transcribe and document orders
Without IVWMS, sterile compounding and infusion preparation are vulnerable to human error. For example, in the case of Eric Cropp and two-year-old Emily Jerry, the pharmacist on duty (Eric Cropp) saw an empty bag and assumed it was the one the pharmacy technician used to mix Emily Jerry’s chemotherapy. Unfortunately, that oversight resulted in the death of Emily, and irreversible consequences for Eric Cropp. If IVWMS technology like Smarthood™ had been around at the time, it would have notified the technician that the sodium chloride scanned in was 23.4% and not the required 0.9%, a teaching moment for the technician and a life-saving catch for Emily Jerry.
The goal of Smarthood™ and other IVWMS solutions is to utilize technology like barcode scanners, EHRs, and medication libraries in the sterile compounding process to eliminate errors in the medication preparation stage. IVWMS solutions have been in progress for over 15 years, and Smarthood™ is a revolutionary product that meets the five key attributes of this technology.
Benefits of IVWMS Technology
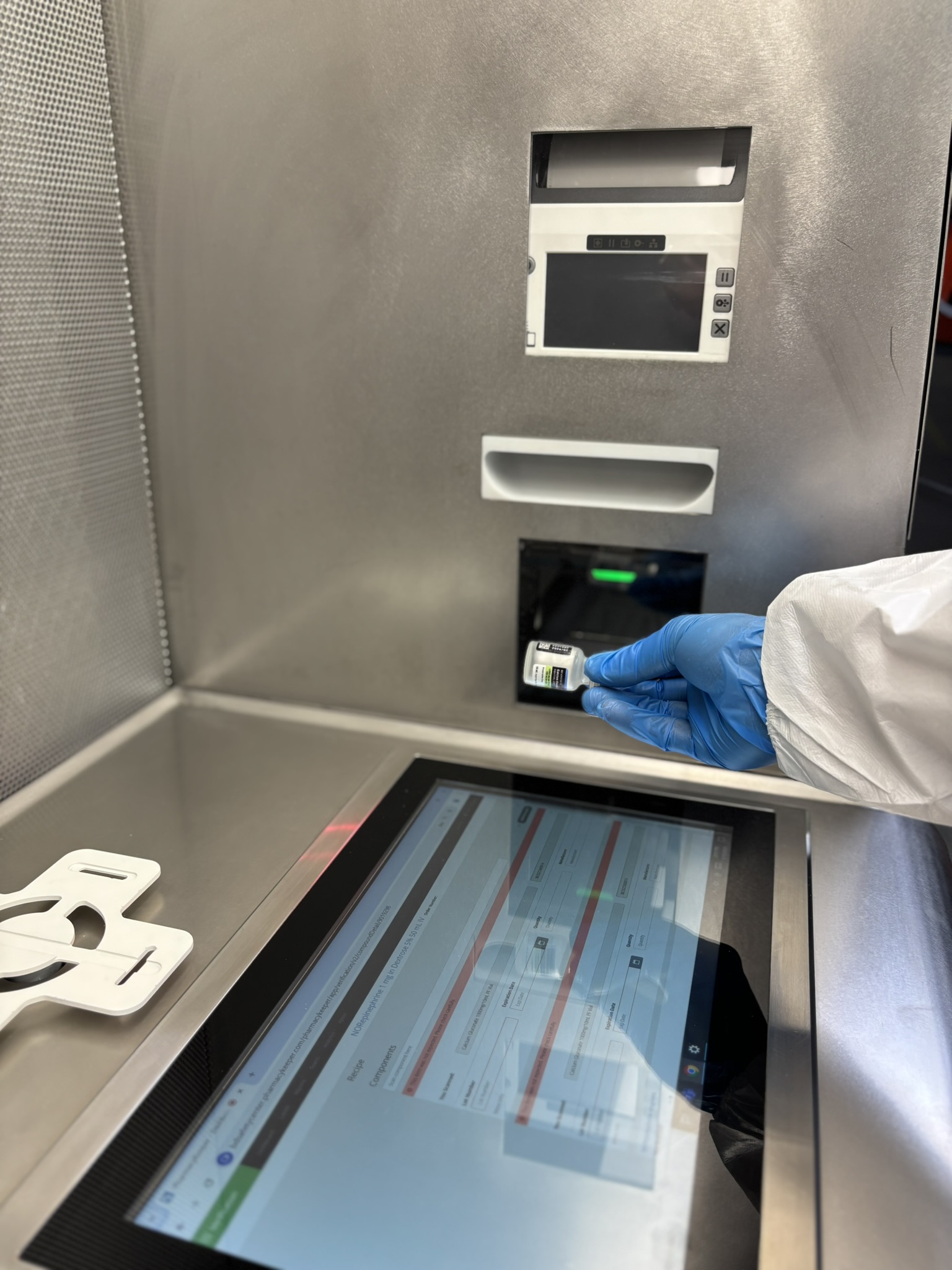 IVWMS technology like Smarthoods™ are designed to be a double-check for clinicians preparing vital medications. They have the ability to prioritize orders based on the time they are due, eliminating early production and disposals of old products. They can also be programmed to alert to certain medications, requiring a pharmacist to verify and approve the ingredients before moving forward in the compounding process.
IVWMS technology like Smarthoods™ are designed to be a double-check for clinicians preparing vital medications. They have the ability to prioritize orders based on the time they are due, eliminating early production and disposals of old products. They can also be programmed to alert to certain medications, requiring a pharmacist to verify and approve the ingredients before moving forward in the compounding process.
 Data collection and reporting can also be incredibly beneficial in the infusion workflow. This technology can measure historical usage statistics and manage drug shortages to reduce waste. Data can also be used to determine opportunities for workflow changes and investigate any errors that are frequently caught.
Data collection and reporting can also be incredibly beneficial in the infusion workflow. This technology can measure historical usage statistics and manage drug shortages to reduce waste. Data can also be used to determine opportunities for workflow changes and investigate any errors that are frequently caught.
Similar to the traditional laminar flow hood, the Smarthood™ also reduces the risks of contamination. By combining technology like barcode scanners, built-in cameras, and filters, it can ensure strict adherence to sterile processes and decrease improper handling of medications or materials. This can aid in standardization of procedures, which has been proven to aid in error reduction and improved clinical outcomes.
An IVWMS solution like the new Smarthood™ is an all-in-one technology workspace that integrates all of the innovative solutions in the medication preparation space to help clinicians achieve the greatest possible results and focus on what matters most—patients.
Challenges
As the Smarthood™ and any other IVWMS technology are all-inclusive solutions to the challenges that plague complex therapies like infusion, they come at a price: the literal price. And while reducing waste and eliminating preparation errors are generous rewards for IVWMS implementation, the cost can be a lofty barrier.
But when using this kind of infusion technology, especially in combination with barcode scanners, vein finder technology, infusion management software, medication libraries, EHRs, and smart infusion pumps—the results speak for themselves.
Technology solutions are the future of many professions, and this extends to healthcare. Particularly when these solutions can be used to enhance patient safety, it is critical that we do what we can to adapt and educate ourselves about the infusion technology available and how it can aid us in providing the safest, most comfortable care for our patients.