Bailey Klingaman compiles a list of resources available for second victims of medication errors, the clinicians. These resources include guidance on supporting individuals with second victim syndrome, explanations on the process of recovery, and details on reporting errors to the appropriate authorities.
With highly-publicized cases like the criminal case of Eric Cropp or the more recent prosecution of RaDonda Vaught, there is no doubt that patient safety and the prevalence of medical errors are serious problems plaguing the healthcare industry.
According to the Institute for Healthcare Improvement, there are “three levels at which damage from errors and adverse events occur: the patient, clinicians, and health care organizations.”
An estimated one in seven patients will be affected by an adverse event in their lifetime according to the Patient Safety Network. Furthermore, nearly half of all clinicians will be involved in an adverse event in their careers.
In a 2007 survey of physicians across the United States and Canada, 92% reported having been involved in a near miss or error event, and 81% reported experiencing emotional distress linked to the incident. This distress is referred to as “second victim” syndrome, and can range in severity from event to event.
What is a medication error?
According to the National Coordinating Council for Medication Error Reporting & Prevention (NCCMERP), a medication error is defined as:
“Any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of the health care professional, patient, or consumer. Such events may be related to professional practice, health care products, procedures, and systems, including prescribing, order communication, product labeling, packaging, and nomenclature, compounding, dispensing, distribution, administration, education, monitoring, and use.”
What is a second victim?
The term “second victim” in reference to healthcare providers was first coined in 2000 by Albert Wu when he wrote, “…although patients are the first and obvious victims of medical mistakes, doctors are wounded by the same errors: they are the second victims.”
This brief definition was later expanded in 2009, classifying a second victim as “a health care provider involved in an unanticipated adverse patient event, medical error, and/or a patient related–injury who becomes victimized in the sense that the provider is traumatized by the event.”
Most recently in 2022, an international group of experts agreed on an evidence-based definition of a second victim: “Any health care worker, directly or indirectly involved in an unanticipated adverse patient event, unintentional healthcare error, or patient injury, and becomes victimized in the sense that also the worker is negatively impacted.”
The American Pharmacists Association unofficially adds to this, clarifying that “second victim syndrome (SVS) is a phenomenon such as when a health care worker harbors feelings of personal responsibility for unexpected patient outcomes and feels that they have failed their patient, going so far as to discredit their own personal knowledge and clinical skills.”
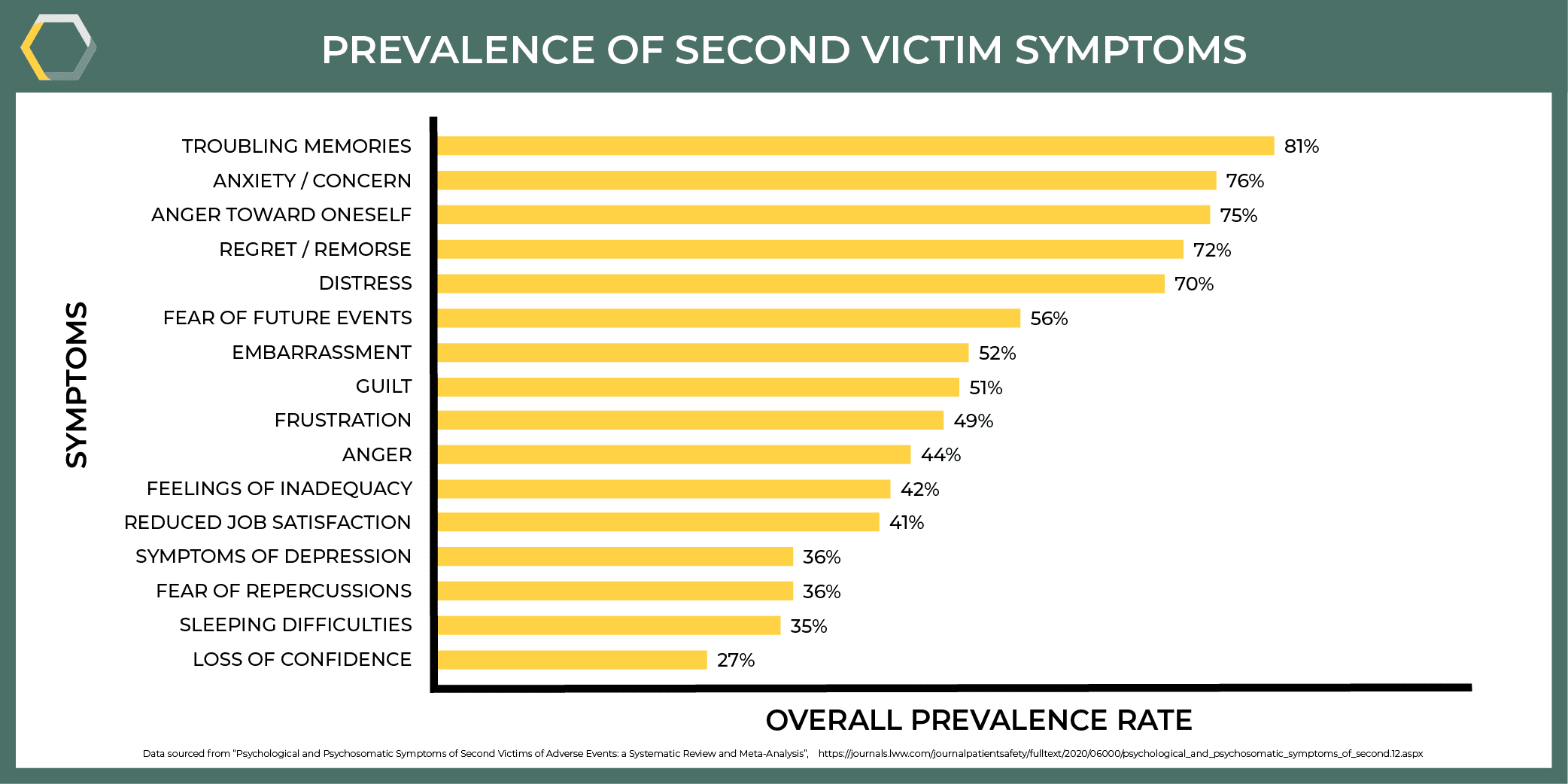
Symptoms of Second Victim Syndrome
While discrediting their personal knowledge and clinical skills is a possibility for those with SVS, it is not a characteristic of all second victims, but rather a potential symptom. Second victims have reported a plethora of anxiety-induced symptoms following an error event, including but not limited to:
- Anger toward oneself
- Regret and remorse
- Distress
- Fear of future errors
- Embarrassment
- Guilt
- Feelings of inadequacy
- Loss of job satisfaction
- Symptoms of depression
- Sleeping difficulties
Seeking Support
Clinicians who have been affected by medical errors or near misses and are impacted by second victim syndrome often rely on the support of those around them: colleagues, friends, family, and their healthcare organization.
Employee Assistance Programs (EAPs)
Employee Assistance Programs, or EAPs, are one of the more common resources available for second victims provided by the healthcare organization. According to the U.S. Office of Personnel Management,
“An Employee Assistance Program (EAP) is a voluntary, work-based program that offers free and confidential assessments, short-term counseling, referrals, and follow-up services to employees who have personal and/or work-related problems. EAPs address a broad and complex body of issues affecting mental and emotional well-being, such as alcohol and other substance abuse, stress, grief, family problems, and psychological disorders.”
However, in a study of interviews with patient safety officers, the Joint Commission found that clinicians are not utilizing EAPs due to the following barriers:
- Accessing the voluntary program requires the clinician to take time away from work and their responsibilities.
- Clinicians are concerned that if they utilize the program, it could be placed on their permanent record and affect them in the future.
- The clinicians have fears or doubts in the confidentiality of the support services.
- They are worried about the negative stigma associated with accessing the program, or receiving judgment from colleagues.
- Clinicians find the support provided in the program ineffective. This is due in part to the program not being designed with second victim syndrome at the forefront.
forYOU – MU Crisis Support
A study conducted by the United Kingdom’s Medical Defense Union found that while nearly half of the clinicians interviewed felt that they received empathy from their colleagues, 67% felt that their healthcare organization did not adequately support them following the event.
And British clinicians are not the only ones feeling this way. The University of Missouri (MU) conducted a survey that found clinicians wanting a department-based support system to aid them after an error has occurred by relieving them of their immediate patient care responsibilities for a brief period; providing support, professional reviews, and constructive feedback; and offering external referrals if necessary.
In response, MU developed a three-tiered program to meet the clinicians needs.
- The first tier involves a department-based team trained in event recognition and basic response training. It is estimated that approximately 60% of clinicians utilizing these services will have their needs met through this tier.
- The second tier consists of peer-support individuals who have been embedded in clinical units to monitor their colleagues for second victim symptoms and intervene if necessary. Approximately 30% of clinicians will have their needs met in this tier.
- The third and final tier is facilitating access to professional counseling. This will meet the needs of the remaining 10% of clinicians involved in the program.
This tiered model is overseen by MU’s forYOU team and has been nationally recognized for its success in supporting caregivers.
What should I do if someone I know made a medication error?
The Johns Hopkins Armstrong Institute published an article in 2015 detailing a comprehensive Do’s & Don’ts list for interacting with a second victim. The following is a synopsis of that article.
Do:
- Bring them away from any commotion that may have ensued.
- Approach them with an open mind and ask an open-ended question to help them process what has occurred.
- Listen and support them, regardless of if you endorse their actions.
- Offer them empathy and understanding.
- Help them identify positive aspects of their life, such as hobbies. Prompt them to plan out the next day with something to look forward to.
- Direct them to resources, like professional counseling or second victim assistance programs.
Don’t:
- Don’t pry into the details of the event or try to determine if they were at fault.
- Don’t try to “fix” the problem or provide solutions.
- Don’t tell the person how the event has made you feel or belittle their emotions.
- Don’t try to tell them how they should or shouldn’t feel. Allow them to process and express their emotions.
- Don’t provide details about your conversation unless absolutely necessary. For instance, if you believe the clinician may be in harm’s way.
What should I do if I made a medication error?
Remain calm and take deep breaths. Providing the patient and yourself with the care needed will be easier if you stay as calm as possible.
Take corrective measures. Communicate the error to the patient’s clinician, the patient, and your immediate clinical supervisor. If you feel overwhelmed, talk to a colleague you trust and ask them for assistance.
Document the incident. Your supervisor may require you to complete an incident report. Be as honest as you can. Try to state the facts of what happened and why it happened without placing blame (on yourself, another clinician, the healthcare organization, etc.). You can also ask a colleague to help you fill out the report if you are in need of support.
Check to see if your state requires medication error reporting to certain bodies. The FDA recommends error reporting regardless of your state, but it is not a requirement. Learn about the reporting law for your state to make sure you’re meeting the requirements.
Seek the support you need. Whether it’s through friends and family, support groups, second victim programs, or an initiative within your organization, don’t be afraid to reach out to those around you for help as you recover.
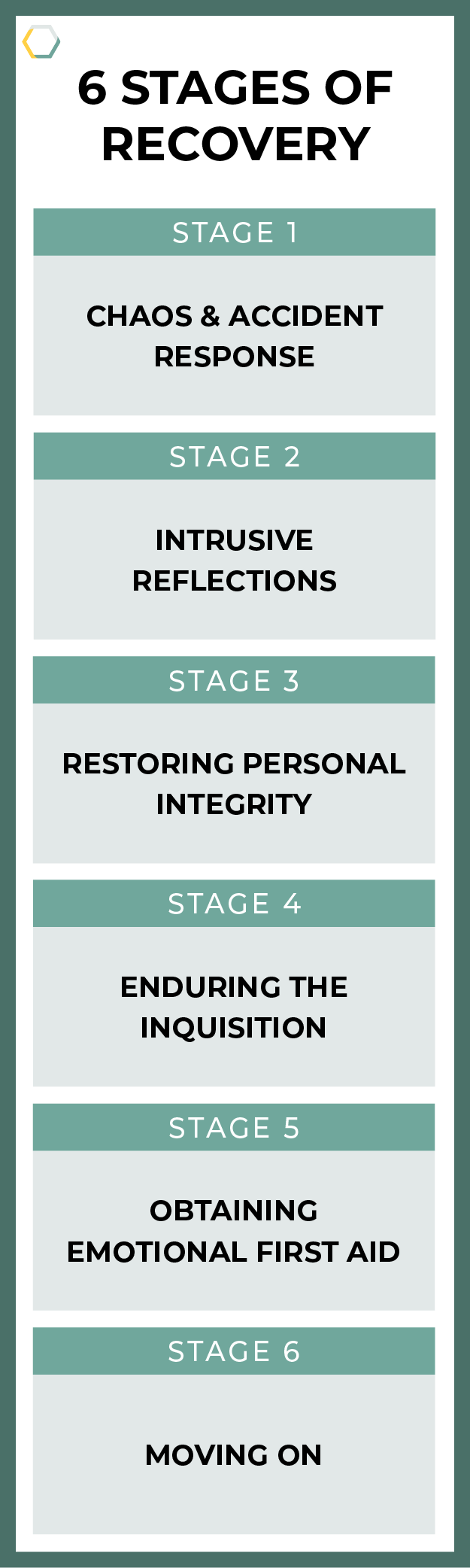
6 Stages of Recovery
There are six stages of recovery for second victim syndrome: chaos and accident response; intrusive reflections; restoring personal integrity; enduring the inquisition; obtaining emotional first-aid; and moving on.
The chaos and accident response stage is when the clinician has learned of the medication error and may be in a state of shock. They may need others to take over the situation while they reflect on the actions that took place.
Following this is the intrusive reflections stage, when the clinician begins to feel the symptoms of second victim syndrome. They may begin to experience grief, guilt, a loss of confidence, or any of the symptoms previously mentioned.
The third stage is restoring personal integrity. This occurs when the clinician seeks support from someone they trust, but is afraid of the responses they may receive.
Enduring the inquisition defines the stage when the clinician prepares for investigation and potential consequences of the event.
The fifth stage involves obtaining emotional first aid. At this point, the clinician feels unsure about who they can confide in, and often feels unsupported.
And the last stage of recovery is moving on. This stage has numerous possibilities and the results are specific to the clinician. Some clinicians may feel unable to return to their position and choose to “drop out” by changing their role, changing practice settings, or changing their profession. For other clinicians, moving on may mean surviving but being unable to forgive themselves. But ideally, with the proper care and resources at their disposal, clinicians may be able to thrive and coax something positive out of the event.
Resources for Second Victims
The following resources are available for those dealing with second victim syndrome:
- Physicians Anonymous is a peer-support group for clinicians. They provide relatable blog posts, one-on-one coaching and mentoring sessions, corporate coaching for organizations, and anonymous meetings where clinicians can meet virtually to support each other in a secure environment. For more information about Physicians Anonymous, see their Frequently Asked Questions.
- The American Pharmacists Association will be creating programs and support groups to provide support to second victims. You can check back on their second victim advocacy page for more information on the availability of programs.
- RxToolKit and our founder, Chuck DiTrapano, have worked with Eric Cropp to create a free webinar educating the industry about second victim syndrome.
How to Report a Medication Error
The FDA does not require medication error reporting, however, it is strongly encouraged to assist in finding solutions. Individual states may have further legislation regarding mandatory error reporting. Be sure to investigate the law in your state to comply with regulations.
For voluntary error reporting, consumers/patients and health professionals can report an error to the FDA’s MedWatch, or to the Institute for Safe Medication Practices’ Patient Safety Organization.