Two years ago, a Nashville nurse was convicted of negligent homicide and impaired adult abuse after accidentally administering the wrong medication to a patient. Read the full facts of RaDonda Vaught’s case, including the support she recieved from hundreds of nurses and how her story sparked change across the country.
In December of 2017, a fatal medication error took place at Vanderbilt University Medical Center. In February of 2019, nurse RaDonda Vaught was arrested for her alleged role in the error and death of a patient, and in March of 2022, Vaught was found guilty of criminally negligent homicide and abuse of an impaired adult.
While these events have undoubtedly affected Vaught personally and professionally, resulting in the loss of her nursing license, a career change, and emotional turmoil – as is common with second victims of medical errors – Vaught’s story offers more than a cautionary tale for clinicians.

What is RaDonda Vaught’s story?
After earning her Bachelor of Science in Nursing from Western Kentucky University in 2014 and becoming a registered nurse, Vaught went on to earn her doctorate in 2015. She spent a year as a nurse at Sumner Regional Medical Center, and in October of 2015 also became a critical care nurse in the neurological/neurosurgical intensive care unit of Vanderbilt University Medical Center, one of the most prominent health systems in Tennessee.
It was at Vanderbilt that Vaught would be involved in a fatal medication error that would dominate the healthcare media and change her life.
The Medication Error
On December 24, two years after Vaught joined Vanderbilt, 75-year-old Charlene Murphey was admitted to the hospital due to a subdural hematoma. After receiving treatment and largely recovering from the brain bleed, Murphey was set to be discharged following a final brain scan.
To calm her before the scan, Murphey was prescribed the sedative VERSED (midazolam), a benzodiazepine used to “relieve anxiety and muscle spasms, and reduce seizures”. Vaught was instructed to retrieve VERSED from Vanderbilt’s computerized medication cabinet and administer Murphey’s dose 1.
According to Vaught’s case, the error was a result of Vaught’s interactions with the medication cabinet. “Vaught attempted to withdraw VERSED by typing ‘VE’ into the system without realizing she should be searching for ‘midazolam,’ the generic name for VERSED 2. When the cabinet did not dispense VERSED, Vaught triggered an override of the machine…”
In overriding the medication cabinet, Vaught procured and administered an injection of vecuronium before leaving Murphey to be scanned. Vecuronium is a nondepolarizing neuromuscular blocker, which is a powerful muscle paralyzer and can have prolonged effects in older populations.
After receiving the paralytic dose, Murphey lost consciousness before suffering cardiac arrest and ultimately being left brain dead. Murphey was kept on a ventilator until her family was able to gather to say their goodbyes, and at 1 a.m. the next day, she was disconnected from the respiratory system 3.
The Aftermath
Realizing what happened, Vaught immediately admitted her error to Murphey’s doctors and hospital officials, taking full responsibility for her part in the error 4. Later that day, Murphey’s death was reported to the medical examiner and deemed a natural outcome of the subdural hematoma, with no mention of the error.
Following Murphey’s death and despite the “natural” cause stated on her death certificate, Vanderbilt negotiated a settlement with Murphey’s family requiring their public silence about her death and the error 4.
In addition to the incomplete reporting on the death certificate, Vanderbilt officials failed to report the error to state or federal officials as is legally required, nor with the Joint Commission which recommends but does not require reporting 5.
Regardless of Vaught’s honesty about her mistake, she was fired from Vanderbilt University in January of 2018. According to her LinkedIn account, Vaught took a “Health and Well-Being” career break for the next few months before starting a position as a critical care nurse at TriStar Centennial Medical Center.
All was quiet, until an anonymous whistleblower notified state and federal officials of the unreported medication error involved in Murphey’s death 4. In response, the Tennessee Department of Health conducted a preliminary investigation and decided not to pursue disciplinary action against Vaught, stating in a letter, “this matter did not merit further action” and Vaught’s case “did not constitute a violation of the statutes and/or rules governing the profession.” 5
However, while the Tennessee Department of Health did not take action, the Centers for Medicare and Medicaid Services (CMS) decided to conduct an investigation at Vanderbilt. This investigation not only confirmed the influence of a medication error in Murphey’s death, but that Vanderbilt failed to report the error to the appropriate authorities. As CMS released its report and findings – without identifying Murphey or Vaught – the error and case quickly became national healthcare news.
In early February of 2019, nearly two months after CMS’s report went public, Vaught was publicly identified when she was arrested for her role in Murphey’s death and charged with reckless homicide and abuse of an impaired adult 1.
The Criminal Trial & Professional Hearing
Later that month, Vaught made her first appearance in court for her criminal case and pled not guilty to all charges. According to an interview with The Tennessean, Murphey’s family forgave Vaught and said that they did not encourage prosecution.
However, Vaught’s forthcoming admittance about her role in the error, as she described herself in her hearing as having been “distracted” and “complacent”, made her defense all the more difficult 1.
Because of the responsibility Vaught had shown, her defense largely relied on identifying and connecting the systemic problems within Vanderbilt that contributed to the error. After her hearing, Vaught’s lawyer insisted that Vanderbilt shared the blame, saying, “There are some real systemic problems with the way they dispense medicine through that automatic dispensing system.” 6

Unfortunately, the immediate facts of the case leaned in the prosecutors’ favor. The investigation into the circumstances surrounding the error alleged that Vaught had made 10 individual errors that resulted in Murphey’s death. These included Vaught overlooking numerous warnings about the medication she pulled from the cabinet, involving a notification directly stating “WARNING: PARALYZING AGENT”.
Following the hearing and at the request of law enforcement, the Nashville Medical Examiner Feng Li was asked to examine Murphey’s death. Aware of the medication error, Murphey’s official cause of death was changed from “natural” to “accidental” 6.
Just over a month after this change in the death certificate, the Tennessee Department of Health rescinded its previous decision not to pursue professional discipline against Vaught, charging her with three infractions: unprofessional conduct, abandoning or neglecting a patient that required care, and failing to maintain an accurate patient record. The consequences of the charges varied from heavy fines to suspension or revocation of Vaught’s nursing license.
Due to the onset of the COVID-19 pandemic, both Vaught’s criminal trial and professional hearing were postponed until July of 2021, when Vaught’s professional discipline hearing finally began.
As was consistent throughout the interviews and statements she made at her legal hearing, Vaught accepted responsibility for her part in the fatal medication error by not double-checking the medication she administered. However, much like her defense in her criminal case, Vaught also argued that the error was possible due to the flaws in Vanderbilt’s system.
While the Tennessee Board of Nursing recognized that there were other issues involved in addition to Vaught’s mistake, Board Vice Chairwomen Amber Wyatt said, “The only thing [the board] is charged with is the mistake that was made by the respondent in front of us today….And when we admit that we’ve done something wrong, it does not dismiss what happened.” 6
So, despite the policy problems within Vanderbilt that contributed to the error and board members appearing sympathetic to Vaught’s case, the board decided to revoke Vaught’s license. She later filed an appeal to get her license back in September of 2021, citing a letter from Vanderbilt’s Director of Medication Safety Terry Bosen, PharmD that “urged the judge to consider that flaws in VUMC’s automated medication dispensing system contributed to the patient’s death.” 4
Nevertheless, Bosen’s letter was not found to contradict the completeness of the board’s record and Vaught’s appeal was denied.
In March of 2022, just over three years after Vaught was arrested for Murphey’s death, her criminal trial began. She was acquitted of reckless homicide, but charged with criminally negligent homicide, a lesser charge under the former. If found guilty, Vaught faced a potential eight years of imprisonment: three to six years for neglect and one to two years for negligent homicide 1.
During her trial, there were testimonies supporting the idea that Murphey’s death was not in fact a result of Vaught’s medication error, but may have occurred as a consequence of her brain injury.

Vanderbilt Neurologist Eli Zimmerman testified that it was “in the realm of possibility” that Murphey’s death was actually completely caused by her condition, and the Nashville Medical Examiner Feng Li testified that while he had determined Murphey’s death to be caused by vecuronium, he was unable to determine how much of the drug she had received and a small dose would likely not have been lethal 1.
Even with these testimonies, the trial ended four days later and found Vaught guilty of criminally negligent homicide and gross neglect of an impaired adult. She was sentenced to three years of supervised probation with judicial diversion (as a first-time offender, her charges could be dropped and her record cleared once probation is successfully completed). The Davidson County Criminal Court Judge Jennifer Smith said that Vaught had faced consequences for her actions and would not be imprisoned unless she violated her probation 2.
Why did this happen?
There are multiple reasons why a medication error that reaches the patient occurs. In this instance, Vaught openly admitted to having been distracted and not double-checking the medication she was administering, while also responsible for orienting a trainee 4.
In an interview in March of 2024, two years after she was found guilty of the charges against her, Vaught spoke up about her responsibility as a clinician. “As a nurse, it falls on me to verify that I have the correct drug. And had I paid close attention, I would have realized that I did not.” 7
At the same time, Vaught also shed light on some of the issues within Vanderbilt that permitted this error to occur. “There were multiple things that could have stopped this along the way had the systems been functioning properly and had the right equipment been in place. There were multiple breakdowns in communication that if they hadn’t occurred, then the need for even having that drug be given in such a hurry would have prevented all of this.”
And Vanderbilt was not the only health system facing staffing and communication issues. The American Nursing Association (ANA) has reported a “nurse staffing crisis”, made worse by the increase of “higher-acuity patients at higher volumes”.
In addition to the high-demand Vanderbilt nurses were facing, Vaught and her lawyer had argued during her trial that one of the main procedural issues that contributed to the error was the lack of communication between Vanderbilt’s pharmacy, the electronic health records, and the medication cabinets. They argued that this caused delays in accessing medications and Vanderbilt’s temporary solution was to override the medication cabinets in order to access the medications faster.
“Overriding was something we did as part of our practice every day. You couldn’t get a bag of fluids for a patient without using an override function,” said Vaught 6.
However, Vanderbilt Director Bosen testified that while the hospital did have technical problems with the medication cabinets, they were resolved weeks before the medication error 1.
Nevertheless, in her recent interview, Vaught chose not to dive deeper into discoveries that had been made in the years following the error, stating, “Honestly, we don’t even have enough time for me to go into the number of things that I have discovered over the four and a half years since Murphey’s death…” 7
What was the response?
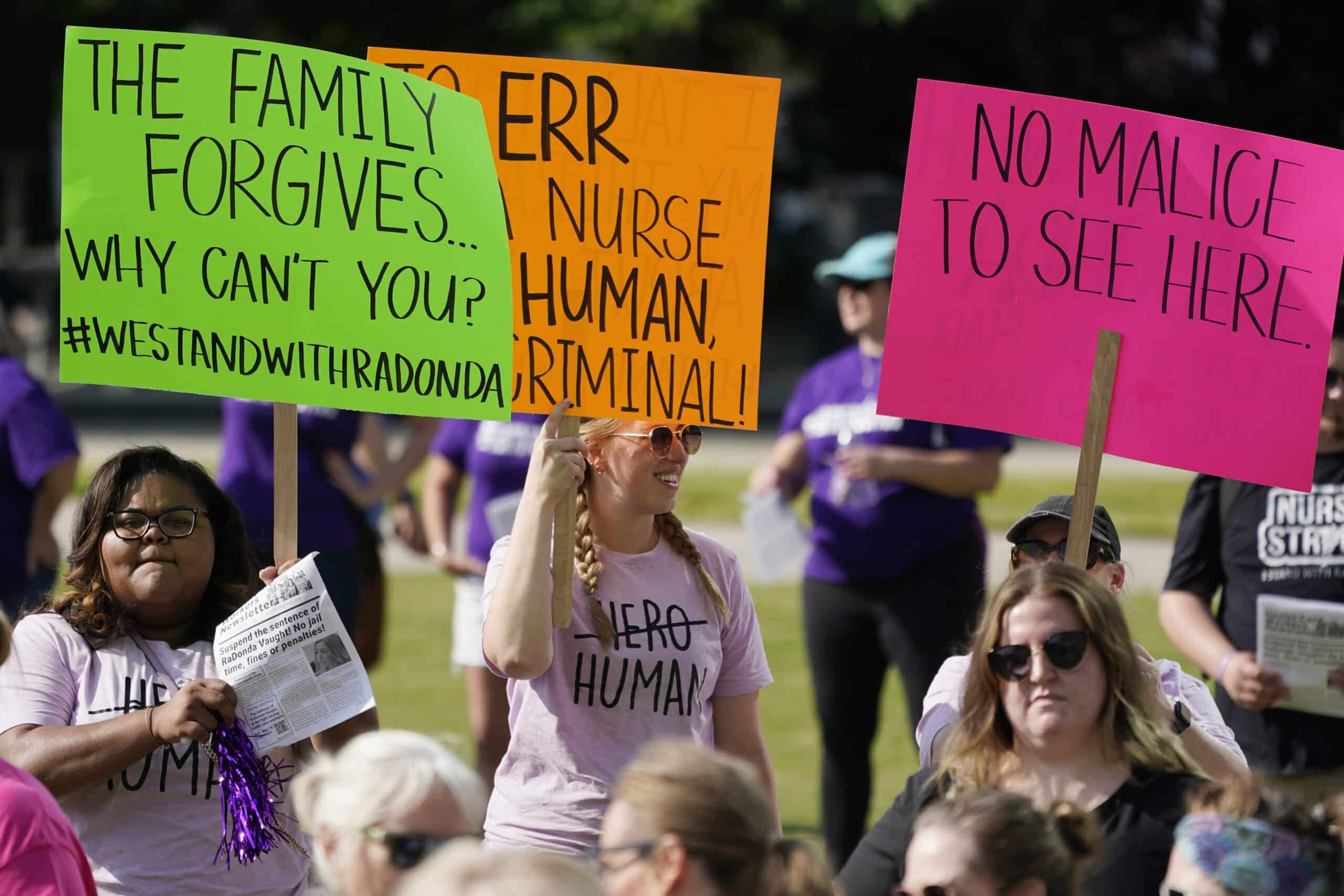
Throughout the incredibly public trial, hundreds of nurses across the country had taken to protesting the criminality of the case, as well as the revocation of Vaught’s license. At the same time, health systems and hospitals were responding as well, triggered by the circumstances at Vanderbilt and the systemic problems that made errors possible at their own institutions.
Vanderbilt
In the immediate aftermath of the medication error before the investigation or trials, Vanderbilt failed to report the error to state officials.
This was confirmed by Vanderbilt Health System CEO C. Wright Pinson during a meeting with the Tennessee Board of Licensing Health Care Facilities. Pinson admitted that the hospital’s response to Murphey’s death and the role of the error was “too limited”, and confirmed the settlement with Murphey’s family 6. The board did not take disciplinary action against Vanderbilt.
After confirming the error and lack of sufficient reporting from Vanderbilt, CMS had threatened to suspend Vanderbilt’s Medicare payments unless the hospital could prove it had taken the necessary steps to prevent a similar error from occurring. To avoid the Medicare suspension, Vanderbilt responded with a “plan of correction”, which The Tennessean obtained through a public records request.
According to Vaught, “At that time it was not required that you reported a death or a sentinel event. What was required is that you have 45 days after such an event to create a corrective action plan….[Vanderbilt] filed their actual amended plan to the CMS report after some number of days. It was over 300 pages. I’ve not seen any new documentation from them.” 7
When asked if there have been any serious repercussions for Vanderbilt in her recent interview, Vaught said, “Not that I know. Vanderbilt has a very good public relations team. They have their own police officers patrolling their campus. They operate as their own little community. They have tremendous resources. But I don’t know what goes on there.” 7
Health Systems
While Vanderbilt was urged to establish its correctional plan, health systems like Hackensack Meridian Health and St. Joseph’s Health have also worked to improve their systems after seeing the consequences of failures at Vanderbilt.
To prevent similar errors with medication dispensing cabinets, Hackensack has adopted the Institute for Safe Medication Practices’ recommendation to require more characters when attempting to withdraw a medication. In 2020, Omnicell updated their medication cabinets to offer this feature as well, and another cabinet company, BD, made this feature a requirement 8.
In addition to taking action to safeguard medications, Hackensack also implemented an error reporting system that connected to its EHR. The introduction of the “Good Catch Program” encourages clinicians to report errors that did not cause moderate or serious harm to patients, and every month recognizes an employee for their good catch.
“If we find and fix the problem while it didn’t cause that kind of harm, we can make sure it does never get to the point where it’s causing moderate to severe harm or death,” said Hackensack VP of Safety & High Reliability Theresa Harris, BSN 8.
Cleveland Clinic reported seeing a steady increase in error documentation, which was attributed to the “system of shared accountability between organizations and employees” it had implemented nine months prior. St. Joseph’s shared this opinion, believing that a true culture of safety stems from every individual’s efforts to build trust among executive leaders, front-line workers, and patients 8.
St. Joseph’s Chief Nurse Dr. Browne believes that trust is maintained through intentional rounding and open communication. By making intentional rounds to the team, Dr. Browne makes each clinician feel heard and that they have an outlet to go to if they are in need of support.
“It takes years to establish a culture of safety and trust in reporting errors, and sometimes it only takes one event such as Ms.Vaught’s case to destroy all the trust that you had built up,” said St. Joseph’s VP of Quality, Patient Safety, and Patient Experience Janine Begasse, BSN, RN 8.
Clinicians & Nursing Organizations
This lack of trust and impending fear is precisely what many clinicians felt after seeing the outcome of Vaught’s trial and discipline hearing. And due to the implications of the case, it was closely monitored by countless nurses and clinicians across the country 1.

During the height of these events, hundreds of nurses rallied behind Vaught, worried that a guilty sentence would set a precedent for the future. In a GoFundMe post to raise money for her defense, Vaught wrote, “Many feel very strongly that setting the precedent that nurses should be indicted and incarcerated for inadvertent medical errors is dangerous.” 6
The ANA released numerous statements regarding Vaught’s trial and professional hearing, expressing concern for what a guilty verdict could mean. If found guilty, nurses feared that this trial meant the increased criminalization of medical mistakes, a decrease in error reporting for fear of repercussions, and nurses becoming the clinical scapegoats for any failures to achieve a culture of safety 2.
ANA President Jennifer Mensik Kennedy, PhD, RN spoke about the inevitably of mistakes and system failures, but that responding appropriately and planning improvements is the best method to effectively prevent repeat errors. “It is inevitable that mistakes happen, and systems fail. Employers must recognize this, and then position their nursing leaders and staff nurses to lead discussions about the right organizational structures to proactively examine errors, develop system improvements and corrective plans.” 8
After the results of Vaught’s criminal trial were publicized, there were mixed feelings from the clinicians who had followed her case. While Vaught had not been imprisoned or sentenced to the full extent of the law, this did not do much to soothe anxiety.
“While we are relieved that Ms. RaDonda Vaught did not receive a prison sentence, we remain disappointed and deeply concerned about the criminalization of error in medicine, which offers no remedy for improving patient safety. In fact, Ms. Vaught’s arrest and conviction makes patients less safe,” the Institute for Healthcare Improvement said in a statement 2.
For any clinicians who have experienced a medication error and are in need of support, you do not need to suffer in silence. The following resources are available to you:
See if your organization offers support services, or implements a Second Victim Support Program.
Read articles providing guidance on accepting responsibility, working through feelings of remorse, and recovery, such as:
-
The Journal of Urgent Care Medicine – Overcoming the Trauma of Making a Medical Error: Self-Forgiveness is an Important Skill for Recovery
-
The American Academy of family Physicians – 5 Ways to Respond to a Medical Mistake
-
Becker’s Hospital Review – What helps physicians after committing a serious medical error? 7 Steps to Recovery


3 Responses
Vecuronium has to be reconstituted.
One thing that is rather obvious is that only generic names of drugs should be used throughout the system. Medicine and pharmacy should both be only using generic names. If the computer only recognizes “midazolam” then the doc would order midazolam, pharmacy would provide midazolam and nurse would administer midazolam