Chuck DiTrapano, RPh and Bailey Klingaman discuss the dangers of distractions and interruptions in the clinical setting, and provide numerous solutions to help reduce the risk of harmful medication errors and improve patient safety.
Anyone who has worked in any healthcare setting can attest to what the Institute for Safe Medication Practices (ISMP) and others have documented: distractions are a major contributor to medication errors.
Why are distractions so dangerous?
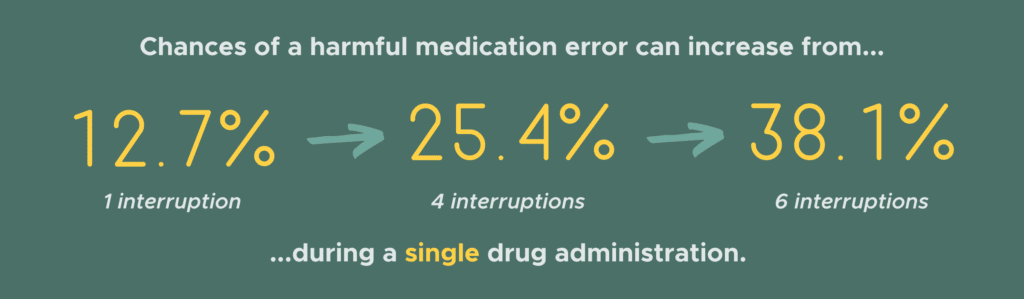
According to the ISMP, the risk of any medication error increases 12.7% with each interruption. The risk of a harmful medication error is doubled when nurses are interrupted four times during a single drug administration, and tripled when interrupted six times.
In addition to the risk of medication errors, distractions can contribute toward inattentiveness, forgetfulness, and inefficiency.
What are the sources of distractions?
Distractions can come from countless directions and have significant consequences.
The ISMP documented an average of one interruption every two minutes in the pharmacy.
Oftentimes, basic methods of communication can actually lead to distraction. The telephone stands as the most prevalent method of communication in healthcare. Voice-activated communication systems such as Vocera are also becoming more popular.
While these tools serve a fundamental purpose, they have the potential to become significant distractions to any healthcare worker.
Phone Calls
Phone conversations, with the exception of conference calls, require a two-way conversation. No one can predict when the phone will ring or when the Vocera will call your name. The caller has no way of knowing if the person they are trying to reach is in a situation where the distraction could prove to be problematic.
Phone calls or Vocera conversations can be considered a “conversational silo”. In most cases, only two people are privy to what is discussed. These types of conversations tend to be repeated over and over again, especially when more than two people or multiple disciplines are involved in a patient’s care. If we don’t want to repeat them, all of the people involved in a patient’s care must have access to prior conversations.
For example, if a nurse calls the pharmacy cleanroom to check on the status of an IV, they cannot know that a different nurse may have just called with the same question. To the IV pharmacist, both phone calls prove to be significant distractions.
Organic Conversations
When preparing or administering an infusion in any ambulatory setting, the potential for distractions can be even greater. In most infusion centers, there will be patients, patient family members, or caregivers and non-clinical staff.
Questions and small-talk with the healthcare worker can distract them, however briefly, from the task at hand. Even hearing background conversations that don’t directly involve the worker can cause them to stray from their task and result in a medication error.
Technology
Most bedside or chair-side nurses work utilizing a computer. Accessing information while working with a patient can present another distraction. Clinical software should allow a nurse in this clinical setting to access all relevant information without the need to open additional windows, use handheld calculators, or seek information from a printed package insert.

Mobile devices in the clinical setting can also be a cause for distraction. In a study regarding smartphone usage during clinical practices, 42.9% of respondents reported having witnessed other clinicians become distracted by these devices.
While mobile devices like smartphones can house clinical software or applications, be used for quick checks, and connect clinicians efficiently, they also have their downsides. Mobile devices have been proven to be distracting in many settings, and healthcare is no exception. App notifications, text messages, and emails are only some of the aspects of mobile devices that cause dangerous distractions.
Just like you shouldn’t be constantly checking your phone while driving, your devices should be silenced, secured, and used only for necessity when it comes to patient care.
Going Off Script
Any good theatrical performance depends on a good script. It’s even more important that everyone in the performance sticks to the script. When someone goes off script, it can be distracting, confusing, and often leads to a bad performance.
If we think of the clinical care provided to a patient, everyone providing the care needs to be on the same script.
For example, you are a patient receiving an infusion. This week the nurse prepares the infusion and administers it using an inline filter. Last week, the nurse did not use a filter.
What do you think? Which nurse is correct? Does it instill confidence? Does it distract you from your care? It may be that both nurses were right, and filtration was optional. But for you, it’s not clear.
Drugs administered in infusion centers do have variability in how they can safely be prepared and/or administered, but that may not matter to the confidence of the patient and can lead to additional questions or distrust in the healthcare industry.
“I’ve always done it that way,” or “I’ve done this many times before”.
The last thing I want to mention is the need to have well-documented and well-utilized procedures to perform any task. Clinicians will sometimes believe that they do not need a written procedure to perform a task, they believe experience negates that need.
If you are following a “mental” procedure and distraction does happen, are you always sure that you haven’t missed a step or confused some aspect of what you are doing? There’s a reason that pilots perform a checklist each time they take off.
Are there solutions to these distractions?
Device Management
There is no doubt that healthcare technology has had—and will continue to have—an incredible impact on the efficiency and accuracy of the industry. But that doesn’t mean having a mobile device management system in place is a bad idea.
Requiring personal devices to be silenced or stored during active work could be the first step toward minimizing non-essential distractions.
Like we said, technology is not the enemy here. Companies like WeInfuse and VirtueScript have been monumental in streamlining healthcare workflows. Innovative software applications like these aren’t your enemy, they’re your best friend.
Clinical Software
To stay focused and attentive to patient needs, a nurse needs a well-designed and complete software application that presents up-to-date, relevant information in a complete, consistent, and concise manner. User experience and satisfaction will intrinsically promote the acceptance and use of clinical software.
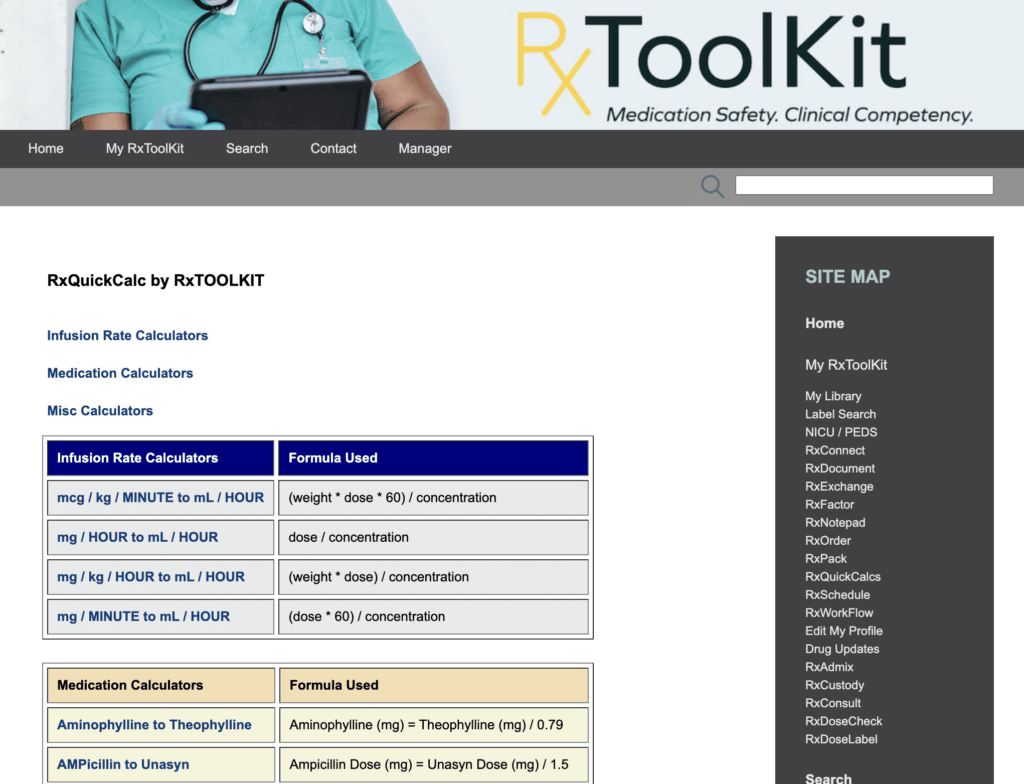
RxToolKit is an excellent example of the ideal clinical software. With over 200 medication guides, product-specific calculators, and instructions for preparation and administration, all essential information is at the tip of your fingers.
Dedicated Distraction-Free Zones
Establishing a secluded or private space to prepare any infusion or injectable drug is important to minimize the interruptions. Not only do distraction-free spaces reduce the opportunity for harmful errors to occur, but they can help with efficiency.
Maximize the potential for productivity by maintaining a clean and organized workspace. “A tidy desk is a tidy mind,” and a tidy mind is a focused and confident worker.
Adaptation and Checklists
Just like the FDA releases updated drug package information, healthcare workers need to adapt their practices to ensure procedure adherence and patient safety.
Each drug should have a script (procedure) and each clinician, regardless of their experience or training, needs to stick to that procedure. Procedure needs to be accessible to all clinicians and reviewed on a regular basis to ensure consistency with that drug’s package insert.
Maintaining a status-quo for drug preparation and administration is about more than habit or experience, it’s about providing the best healthcare for the patient.