In the past two decades, patient safety has become a prevalent issue in our healthcare industry despite the introduction of numerous methods to combat medication errors and preventable harm. Led by a coalition advocating for change, the solution to the patient harm problem has been discovered: the creation of a National Patient Safety Board.
Patient safety has been a recognized national issue since the release of the “To Err is Human” report by the Institute of Medicine in the late 90s. However, despite the technological advancements and scientific discoveries that have taken place over the last 25 years, medication errors and safety in healthcare are still present challenges.
The industry is now calling for a new solution, one that has proved successful in other countries to reduce preventable errors and inspire patient safety culture: the establishment of a national patient safety board.
The Problems with Patient Safety
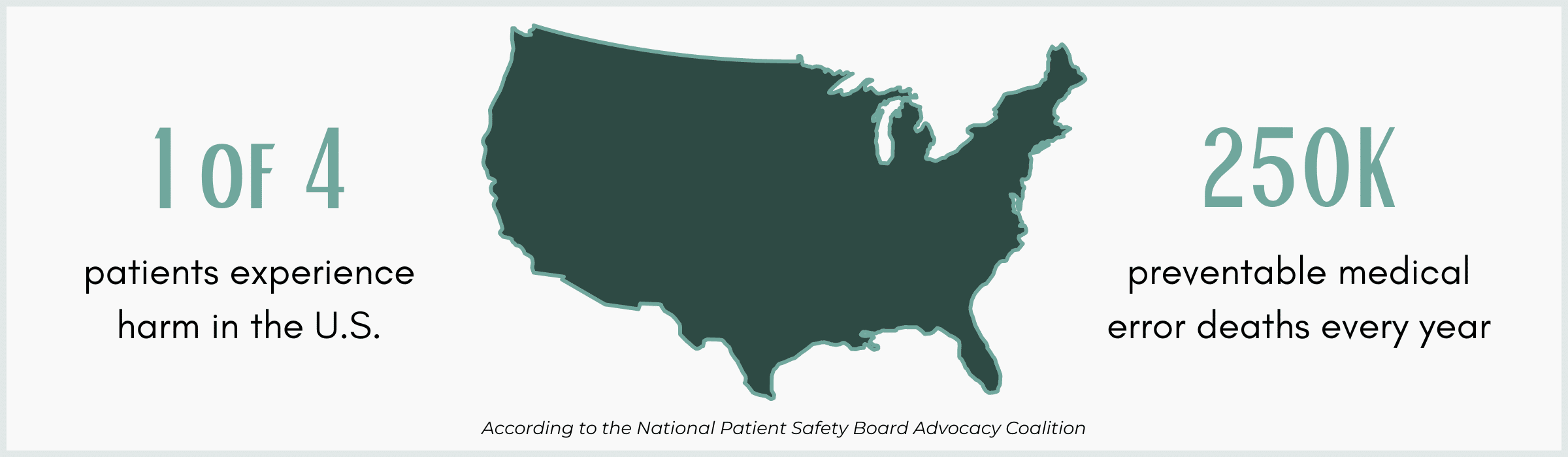
In the “To Err is Human” report from 1999, an estimated “44,000–98,000 patients die from preventable errors in American hospitals each year,” a number that has only grown over the past two decades. Current studies reflect that approximately 400,000 patients experience some form of preventable harm in hospitals each year, and more than 200,000 patients die from medical errors.
Furthermore, due to workforce shortages, clinician burnout, the surge in patients requiring care, and supply chain shortages, the recent COVID-19 pandemic contributed substantially to patient and clinician safety challenges.
The Patient Safety Network attributes this decline partially to the overreliance on healthcare workers to maintain safety among the other responsibilities and stressors of their job. While there have been new methods and proposed solutions to the patient safety problem, many of these fall solely on the shoulders of clinicians without providing wide-spread, systemic solutions.
Recommendations for Improvement
Patients for Patient Safety US
In January of 2023, the Patients for Patient Safety US (PFPS US) organization released a statement commenting on what the network believed to be the root of the patient safety problem: a lack of federal accountability. PFPS US called for the U.S. Department of Health and Human Services (DHHS) and the National Healthcare System Action Alliance to establish federal leadership focused on patient safety.
PFPS US stated, “In the absence of committed and coordinated leadership, patient safety has drifted as a national priority, become marginalized and has been positioned, alarmingly, as competitive with other priorities, such as worker safety or health equity.”
The organization recommended the following to counteract the deterioration of patient safety:
- Patient safety should be reinstated as a national priority in the DHHS healthcare strategy.
- DHHS should establish a Federal Advisory Committee to facilitate communication and efforts across federal agencies to oversee the safe delivery of healthcare services and products.
- DHHS should establish an independent organization responsible for analyzing data, conducting investigations, providing patients and clinicians with an outlet to report patient safety harm, and making recommendations to stakeholders to enhance safety efforts.
- DHHS should invest in patient safety initiatives, promote accountability, and apply consistent and appropriate consequences for failing to report harmful events.
President’s Council of Advisors on Science and Technology
 At the executive level, the President’s Council of Advisors on Science and Technology (PCAST) submitted a report to the office of the president in September of 2023, also suggesting federal leadership to prioritize patient safety. (Note: As of January 2025, this report is no longer available on the White House’s website.)
At the executive level, the President’s Council of Advisors on Science and Technology (PCAST) submitted a report to the office of the president in September of 2023, also suggesting federal leadership to prioritize patient safety. (Note: As of January 2025, this report is no longer available on the White House’s website.)
In this report, the Council urged the President to establish a “White House-led” initiative to “solve the critical challenges with patient safety in the public and private sectors” as soon as possible. “We now need federal government leadership to create a nationwide transformational initiative on patient safety to support every hospital and practitioner with implementing these solutions and sustaining them over time.”
This initiative would involve 1) the appointment of a Patient Safety Coordinator responsible for the cooperation of all relevant government agencies, and 2) the establishment of a multidisciplinary National Patient Safety Team comprised of individuals from highly-affected populations.
Safety Initiatives in Action – International
The issue of ensuring patient safety is not a challenge the U.S. faces alone. However, organizations based in the U.K., Norway, and Finland are examples of national patient safety boards in action. These organizations have demonstrated the successful application of a federal body responsible for patient safety initiatives.
England – Health Services Safety Investigation Body
England’s Health Services Safety Investigation Body (HSSIB) was established in 2023 to “investigate patient safety concerns across the NHS in England and in independent healthcare settings where safety learning could also help to improve NHS care.”
The HSSIB reduces medical harm by:
- Encouraging the involvement of patients, families, and clinicians in healthcare
- Supporting healthcare workers in their responsibilities and the safe care of patients
- Creating safer healthcare environments and processes
- Promoting efficiency in the healthcare industry
- Sharing best practices and innovative solutions
Norway – Healthcare Investigations Board
Formed in 2019, the Norwegian Healthcare Investigation Board (NHIB) investigates adverse events and errors in the healthcare industry in order to identify factors that can contribute to patient harm. Its investigations involve the caregivers, patients, and families for transparency and inclusivity. The goal of the NHIB is to improve patient safety by facilitating an environment of trust and education.
Finland – Safety Investigation Authority
The Safety Investigation Authority of Finland (SIAF) was founded in 1996 as an impartial and independent body responsible for investigating events across the aviation, railroad, marine, health, and social sectors. The investigative team examines the event for causes, actions taken, and consequences for the purpose of prevention.
The duties of the SIAF include:
- Monitoring the safety investigation
- Maintaining cooperation connected with safety investigations
- Issuing safety recommendations
- Monitoring the implementation of said recommendations
National Patient Safety Board – United States
Taking action for patient safety in the United States and inspired by successful international programs, a collection of companies and organizations (including RxToolKit) have assembled under an Advocacy Coalition proposing the creation of a National Patient Safety Board (NPSB).
Consisting of healthcare organizations, provider associations, nonprofit organizations, advocacy groups, and businesses in the healthcare industry, the Advocacy Coalition supports the establishment of the NPSB and meets to discuss strategies on progressing the proposal.
What is the National Patient Safety Board?
The National Patient Safety Board was first proposed to the House of Representatives in 2022 as the National Patient Safety Board Act (H.R. 9377). In March of 2024, California Representative Nanette Barragán and Texas Representative Dr. Michael Burgess, members of the Energy and Commerce Subcommittee on Health, reintroduced the act as H.R. 7591.
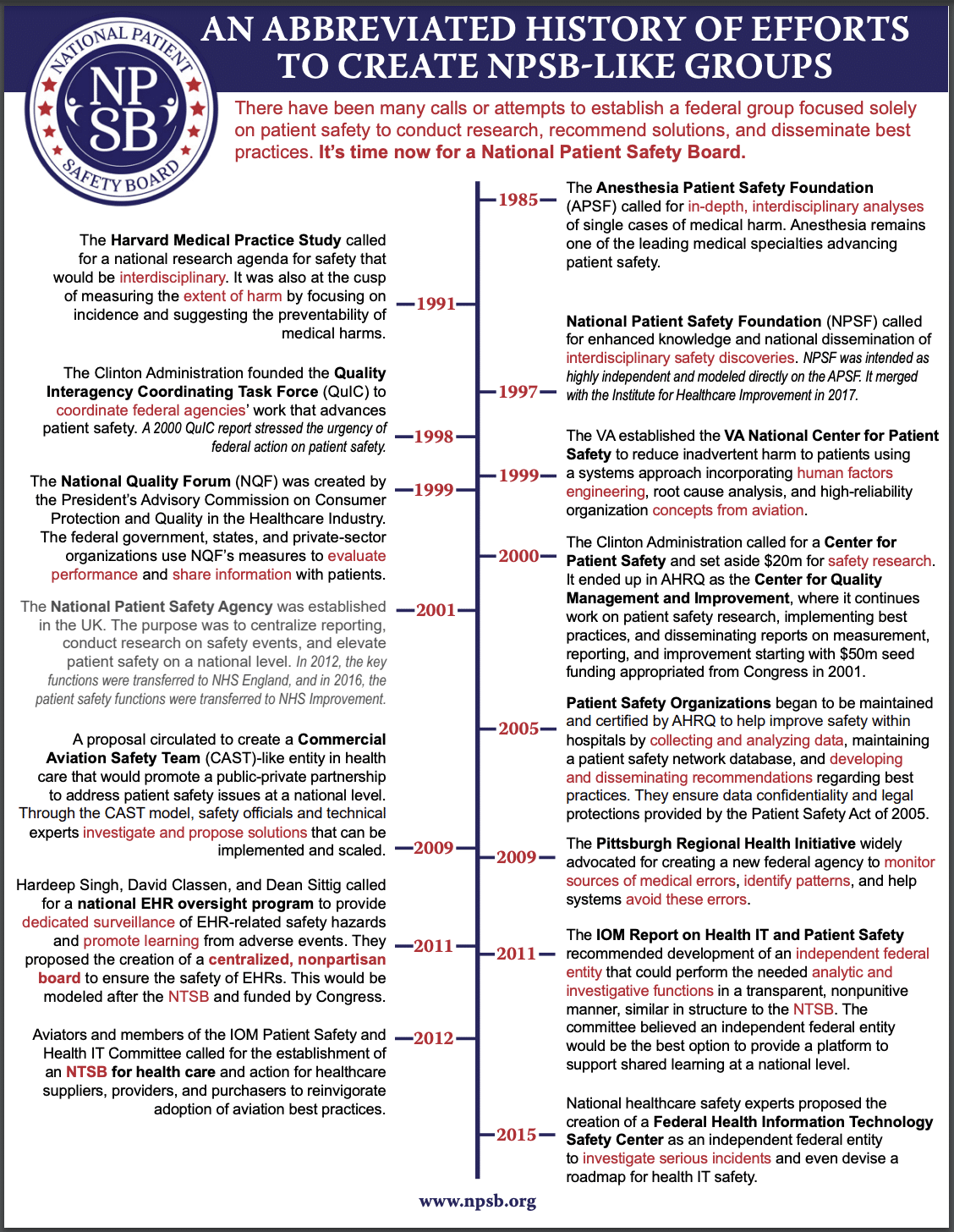 The creation of the National Patient Safety Board has been a dynamic idea dating back to 1985 when the Anesthesia Patient Safety Foundation called for an analysis of medical harm cases. Since then, the United States has seen the creation of the National Patient Safety Foundation (NPSF), the Quality Interagency Coordinating Task Force, the Center for Quality Management and Improvement, the Federal Health Information Technology Safety Center, and more agencies/foundations designed to solve the patient safety issue.
The creation of the National Patient Safety Board has been a dynamic idea dating back to 1985 when the Anesthesia Patient Safety Foundation called for an analysis of medical harm cases. Since then, the United States has seen the creation of the National Patient Safety Foundation (NPSF), the Quality Interagency Coordinating Task Force, the Center for Quality Management and Improvement, the Federal Health Information Technology Safety Center, and more agencies/foundations designed to solve the patient safety issue.
However, the proposed NPSB would be slightly different from these organizations. The NPSB would be modeled after the Commercial Aviation Safety Team (CAST) and the National Transportation Safety Board (NTSB), two organizations that have successfully implemented and maintained safe practices in the transportation industry.
Like CAST and the NTSB, the National Patient Safety Board would identify and anticipate causes of preventable harm, provide recommendations and solutions to eliminate these causes, and propose non-punitive reactions to patient safety events (unlike the criminal repercussions that former pharmacist Eric Cropp faced, or the disciplinary hearings former nurse RaDonda Vaught experienced).
The Board’s Responsibilities
The primary purpose of the National Patient Safety Board would be to create solutions that eradicate preventable patient safety events. According to the NPSB, a patient safety event is defined as:
- an action or inaction that led to a patient injury or harm in a healthcare setting,
- an action or inaction that could lead to patient injury or harm as precursors to potential harm in a healthcare setting, or
- a near miss that could have harmed the patient but did not cause harm in a healthcare setting as a result of chance, prevention, or mitigation.
In order to prevent these patient safety events from occurring, the National Patient Safety Board would be designed to close the gap between current initiatives and organizations.
What the NPSB will and won’t do:
The National Patient Safety Board would not collect any additional data, but would monitor and examine pre-existing data sources to determine causes of harm. There are many current sources of data that reflect the preventable harm in healthcare, but the data is not being analyzed to determine the causes and solutions to these events. The NPSB would examine the data with the goal of identifying the problem areas and proposing solutions.
The National Patient Safety Board would not publicly report data, or certify, accredit, regulate, or license healthcare organizations. Similarly, the NPSB would not be authorized to enter organizations and perform its own investigations of patient safety events. Instead, the Board will provide organizations with a team of experts, including “clinically-informed human factors engineers”, to assist the organization in identification of the causes and implementation of solutions.
The Board would establish a Healthcare Safety Team to operate as a public-private group dedicated to finding solutions to preventable patient harm on the national scale. There is currently no single entity responsible for identifying patterns of harm and deducing resolutions.
The Benefits of the NPSB
In April of 2023, Committee Lead for Patients for Patient Safety US’s National Patient Safety Oversight Committee Olivia Lounsbury published an article commending the National Patient Safety Board.
She wrote that the NPSB would benefit patients, families, and the public through its complementary foundation. Rather than establish another agency that determines patient safety issues, the NPSB would complement existing organizations and work to fill the gaps to bring positive action.
The NPSB would be designed to incorporate the voices of patients and family members, so those directly impacted by safety events have a seat at the table and are included in innovative discussions.
The National Patient Safety Board Advocacy Coalition has also released a comprehensive document laying out the benefits of the NPSB for patients and families, stating the following:
- The NPSB, with the sole mission of improving patient safety, will give patient safety a federal home, ensure coordination of patient safety efforts, and serve as the centralized point of contact for patient safety-related challenges.
- The creation and existence of the NPSB sends a strong message to health providers and administrators that safety is a top national priority.
- The NPSB Act requires the integration of patient and family representatives at the top governance level where priorities are set.
- The NPSB may also have the power to examine certain cases to further understand early indicators of patient safety risks.
- The NPSB will feature a reporting portal that will provide a new pathway for patients, healthcare staff, and others to report data and concerns about healthcare-associated risks, harms, or injury, which would otherwise remain uncollected.
- Along with patient safety reports, the NPSB will have access to a large dataset of injuries and harms that occur in health care. Therefore, these events will have a much greater likelihood of being identified quickly and even anticipated before they happen with artificial intelligence.
- NPSB’s data and information will be analyzed and used to inform research, develop solutions, and make recommendations for stakeholders responsible for ensuring safety, for example State departments of health, professional licensing boards, accreditors, Federal agencies, and healthcare providers to prevent harm and injury from reoccurring in healthcare settings across the U.S.
- To gain consensus on the solutions that need to be adopted, the NPSB would have a multi-disciplinary, public-private healthcare safety team with patient and family representatives on the team. This process creates buy-in, increasing the likelihood that the solutions would be adopted by health systems, federal agencies, and other stakeholders in the private and public sectors to fix the systemic causes of safety risks.
How to Get Involved
To learn more about the National Patient Safety Board or to show your support, visit npsb.org.