In this article, Dr. Jill Paslier, PharmD, CSP, FISMP discusses the growth of specialty infusion pharmacy and the increasing demand for pharmacists. She covers the challenges in hiring and training for the infusion setting, and provides a framework for enhancing training to ensure success for pharmacy teams.
Infusion therapy is increasingly used to treat chronic illnesses, a population projected by the National Institutes of Health (NIH) to nearly double in the U.S. over the next 30 years. Advances in infusion drugs and delivery methods have expanded access and utilization. At the same time, payers are driving a shift from costly hospital settings to lower-cost sites of care, such as patients’ homes. In response, hospitals and clinics are developing infusion programs to expand capacity and retain revenue. 1
This growth has created a rising demand for specialty infusion pharmacists, but there are too few with the necessary expertise in biologics, rare diseases, benefit navigation, and infusion handling. Because of these specialized skill requirements, onboarding often takes longer and comes with a steep learning curve.
This article will explore challenges in recruiting experienced specialty infusion pharmacists and offer strategies to overcome them—such as identifying transferable skills, key professional qualities, and remote role options. It will also present a structured framework to train generalist pharmacists into competent specialty infusion pharmacists.
Challenges in Hiring Experienced Specialty Infusion Pharmacists
Pharmacy education and training pathways have not kept pace with the rapid growth of specialty infusion pharmacy. Most pharmacy schools offer limited exposure to specialty infusion therapies and related disease states, and few have faculty with direct experience in this area. As a result, students often graduate with little understanding of specialty infusion pharmacy until they encounter it during postgraduate training or on-the-job experience. 2
Formal training opportunities are also limited. A 2016 survey found that only 17% of U.S. pharmacy schools offered a specialty pharmacy track, and as of July 2024, there were just 51 accredited postgraduate year one (PGY-1) and PGY-2 specialty pharmacy residencies nationwide, with even fewer focused on infusion. 2,3 Among practicing specialty pharmacists, nearly half of health-system leaders reported that fewer than 30% of their pharmacists had completed a residency, though about 60% held the Certified Specialty Pharmacist (CSP) credential. 4
These data reveal a major training gap. Without stronger educational pathways, mentorship, and structured onboarding programs, the specialty pharmacy workforce will continue to rely heavily on experiential, on-the-job learning.
Transferable Skills and Key Qualities
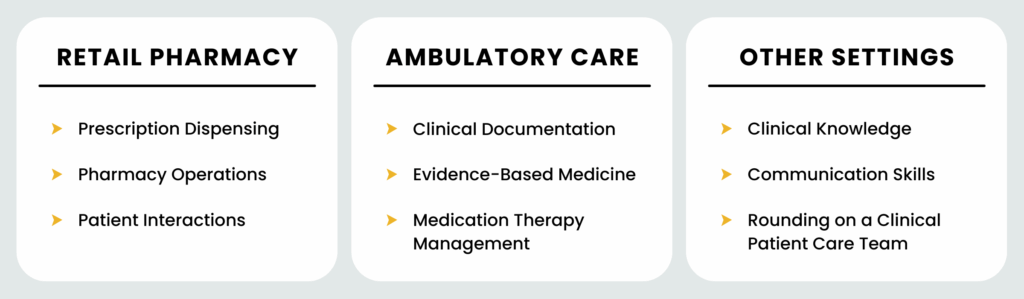
Addressing the workforce gap begins with identifying the right candidates for specialty infusion roles and recognizing the skills that translate well to this complex practice area.
Because direct specialty pharmacy experience is uncommon, employers can focus on transferable skills that provide a strong foundation for success. Retail pharmacy experience, for example, builds essential competencies in prescription processing, operations, patient communication, and medication counseling. Pharmacists with ambulatory care experience bring additional strengths in medication therapy management, clinical documentation, laboratory review, and evidence-based decision-making. While they may need further disease-specific training, their clinical reasoning skills and familiarity with guideline-based care allow for faster adaptation to specialty workflows.
Experience in multidisciplinary care settings is also valuable. Pharmacists who have participated in patient rounds or collaborated with clinical teams often demonstrate sound judgment, clear communication, and the ability to manage complex patient cases—skills that directly translate to specialty pharmacy practice.
In addition to professional experience, certain personal qualities are important predictors of success. Adaptability, curiosity, and a strong desire to learn are essential, given the rapid evolution of specialty infusion medications and workflows. Effective communication skills support both patient counseling and collaboration with healthcare providers. Emotional intelligence and teamwork foster resilience and contribute to a positive, high-performing workplace culture. Equally important is a high attention to detail and a dedication to consistent documentation across workflows, ensuring accuracy, continuity of care, and compliance with clinical and accreditation standards.
While technical expertise remains important, the combination of transferable skills, clinical judgment, and key personal attributes often determines how well a pharmacist transitions into and thrives within specialty infusion pharmacy. Structured onboarding and training programs can then build on this foundation to develop full specialty infusion competency.
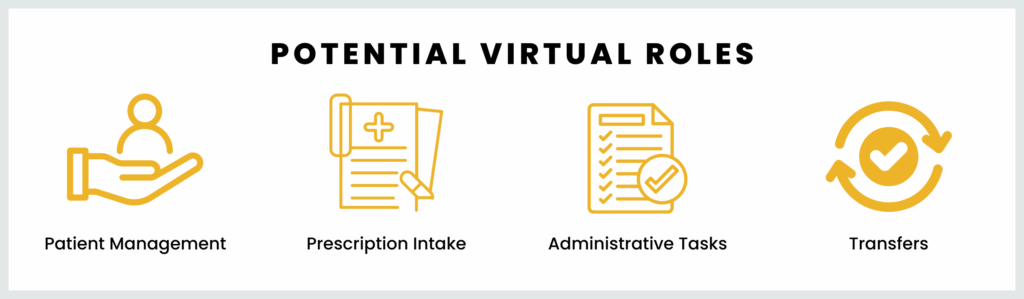
Virtual Roles
An effective strategy for addressing workforce shortages is expanding the use of virtual or hybrid roles within specialty infusion pharmacy. When supported by secure systems and state regulations, remote work can greatly widen the candidate pool—especially for experienced or hard-to-find talent.
Virtual roles are well suited for non-dispensing tasks such as patient assessments, clinical reviews, counseling, prescription processing, prior authorizations, insurance coordination, and administrative functions. These positions can be performed remotely when proper technology and safeguards are in place.
According to a recent ASHP survey, 82% of health system specialty pharmacies use a hybrid model, 16% remain fully on-site, and only 2% operate entirely remotely. Most teams conduct training in person but provide remote access to operational systems, supported by clear remote work agreements. Notably, 94% of staff and leaders reported positive experiences with remote work, citing fewer distractions, better focus, and improved flexibility. 5
Allowing virtual positions can help attract qualified talent from across the country, improve retention, and strengthen specialty infusion pharmacy teams in a challenging hiring market.
Orientation and Training Curriculum
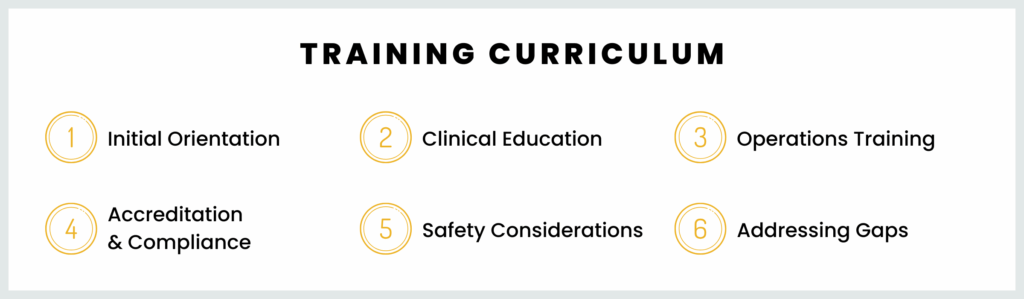
A strong specialty infusion pharmacist training program should include six main components: initial orientation, operations training, clinical education, accreditation and compliance, patient safety, and addressing gaps. 6,7,8
The programs below offer valuable insights and examples of best practices in these areas. Links to each are provided in the Supplemental Resources section at the bottom of this article.
- American Society of Health-System Pharmacists (ASHP) Specialty Pharmacy Certificate
- ASHP Compounded Sterile Preparations Certificate for Pharmacists
- National Association of Specialty Pharmacy (NASP) Certified Specialty Pharmacist (CSP) Prep Course
- The National Home Infusion Association (NHIA) Sterile Compounding Advanced Certificate Training
- RxToolKit RxELearning
- Specia Tutor disease-specific educational resources
Initial Orientation
Initial orientation should cover policies, procedures, privacy, regulatory and compliance requirements, and generally all topics required by accreditation.
Clinical Education
Clinical training should then focus on disease-state education, evidence-based guidelines, and medication-specific details such as dosing, side effects, Risk Evaluation and Mitigation Strategies (REMS), and counseling points. Training should also include patient assessment and documentation skills as required by accreditation, supported by accessible reference tools. 6,7,8
Operations Training
Operations training should cover core dispensing workflows, infusion product preparation and sterile compounding techniques (including USP 797), provision of infusion supplies, shipping logistics with temperature control procedures, and strategies to prevent errors (including USP 659). Reviewing actual near misses or past errors reinforces safety practices and strengthens accountability. 7,8,9
Accreditation and Compliance
Accreditation and compliance training should explain the purpose behind accreditation standards specific to your organization. Clinicians should understand how documentation, follow-ups, and quality metrics support regulatory compliance and patient safety.
Patient Safety
Patient and medication safety education should include high-risk medication precautions and emergency response procedures. Incorporating best practices from the Institute for Safe Medication Practices (ISMP) and reviewing external error reports helps build a proactive safety culture. 6,7,8,9
Addressing Gaps
Finally, supplemental training may be needed in documentation, phone etiquette, and patient communication—especially for clinicians from non-patient-facing settings. Emphasizing empathy, professionalism, and cultural sensitivity prepares pharmacists to provide high-quality, patient-centered specialty care.
Training Materials and Tools
Training materials and tools are essential to help clinicians develop consistency and confidence in specialty infusion pharmacy practice.
Foundational resources should include drug cards and mini-monographs summarizing key clinical and safety information. These must be kept current, as ISMP has identified outdated references as a frequent cause of medication errors. All staff should use standardized, regularly updated materials. 10
Comprehensive drug information databases such as Pyrls, Lexicomp, or Micromedex should be integrated into training and daily practice to support evidence-based decision-making. For infusion-specific content, resources like RxToolKit and Specia Flow can provide targeted references and disease-specific clinical reviews. 6
Competency assessments and training checklists further support structured learning. Knowledge checks can cover disease states or operational skills, while detailed task-based checklists—such as those for medication packaging and shipping—ensure each step is completed correctly. 11
Finally, regular oversight and audits reinforce quality and compliance. Reviewing patient documentation, including Medicare Part B records, and conducting call audits help verify accuracy, professionalism, and adherence to accreditation standards. 11
Conclusion
Building a skilled specialty infusion pharmacy team requires more than finding experienced candidates—it depends on creating a thoughtful, structured training and onboarding program. By identifying transferable skills, emphasizing clinical education, reinforcing operational excellence, and instilling a culture of compliance and safety, pharmacies can transform motivated clinicians into confident specialty infusion professionals.
As the demand for infusion services continues to rise, investing in education, mentorship, and robust training tools not only strengthens workforce readiness but also enhances patient outcomes and operational quality. With the right framework in place, every new hire has the potential to grow into a capable, compassionate specialty infusion pharmacist equipped to deliver the highest standard of care.
Supplemental Resources
- ASHP Specialty Pharmacy Certificates
- ASHP Compounded Sterile Preparations Certificate for Pharmacists
- NASP CSP Certification Exam Prep Course
- NASP University
- NHIA Sterile Compounding Advanced Certificate Training
- RxToolKit RxELearning
- Specia Tutor disease-specific educational resources
- Connect with specialty pharmaceutical representatives for more educational opportunities.
1 Infusion Therapy Market Overview. Mertz Taggart. 2024. https://infusioncenter.org/wp-content/uploads/2024/06/Infusion-Industry-Overview.pdf
2 Islam M, Chen G, Talukder R. Specialty tracks in Pharm.D. curricula of US colleges and schools of pharmacy. Currents in Pharmacy Teaching and Learning. 2016. https://www.researchgate.net/publication/308388593_Specialty_tracks_in_PharmD_ curricula_of_US_colleges_and_schools_of_pharmacy
3 Specialty Pharmacy Focused Residency Programs. ASHP. July 7, 2024. Accessed April 18, 2025. https://www.ashp.org/specialty-pharmacy-practitioners/specialty-pharmacy-focused-residency-programs
4 Kelley T, Canfield S, Diamantides E, Ryther A, Pedersen C, Pierce G. ASHP Survey of Health-System Specialty Pharmacy Practice: Practice Models, Operations, and Workforce — 2022. American Journal of Health-System Pharmacy. 2023;80(24):1796-1821. doi:https://doi.org/10.1093/ajhp/zxad235
5 Results of the Health-System Specialty Pharmacy Work-from-Home Survey: Part 1. American Society of Health-System Pharmacists (ASHP). July 1, 2025. Accessed July 8, 2025. https://www.ashp.org/professional-development/ashp-podcasts/hot-topics-in-pharmacy-practice/2025/results-of-the-health-system-specialty-pharmacy-work-from-home-survey-part-1?loginreturnUrl=SSOCheckOnly
6 Better Care. Better Outcomes, Lower Costs. Specia. 2025. Accessed July 6, 2025. www.speciarx.com
7 CSP Exam Prep Course. National Association of Specialty Pharmacy (NASP). ND. Accessed July 6, 2025. https://naspnet.org/csp-prep-course
8 Specialty Pharmacy Certificate. ASHP. 2025. Accessed July 6, 2025. https://www.ashp.org/professional-development/professional-certificates/specialty-pharmacy-certificate
9 Institute for Safe Medication Practices (ISMP). ISMP Targeted Medication Safety Best Practices for Community Pharmacy. ISMP; 2025.
10 Institute for Safe Medication Practices. Spotlight on the Key Elements of the Medication System – Part 1. ISMP Medication Safety Alert! Community/Ambulatory Care. 2003;2(10):3-4.
11 Skilton L, Bolster L, Background C. Highlighting the Benefits of a Personalized Onboarding Program for Clinical Pharmacists with Diverse Work Experience. Shields Health Solutions. 2024. https://shieldshealthsolutions.com/content/uploads/2024/10/NASP-2024_CPED-Poster_FINAL-8.19.24.pdf
About the Author: